How Fermented Foods, Fiber, and Probiotics Support Your Gut Microbiome: Organic Gut Health Supplement Guide
The human gut microbiome represents one of the most complex and influential ecosystems in the body, profoundly affecting overall health, immunity, and even mental wellbeing. [1] Recent scientific advances have revealed that gut health extends far beyond simple digestion, playing critical roles in immune system regulation, metabolic function, and disease prevention. [2] This comprehensive guide explores evidence-based strategies for optimizing gut microbiome diversity and function through diet, supplementation, and lifestyle modifications.
| Key Takeaways |
|---|
|
Understanding Gut Health and the Microbiome
The gut microbiome comprises trillions of microorganisms residing in the gastrointestinal tract, forming a complex ecological community that profoundly influences human physiology. [1] Research has established that microbiome composition varies significantly between individuals based on factors including diet, geography, age, and genetics. [9] Importantly, greater microbial diversity generally correlates with improved health outcomes, while reduced diversity has been associated with various chronic conditions including obesity, inflammatory bowel disease, and metabolic disorders. [3]
The Role of a Balanced Gut Microbiome
A balanced gut microbiome performs multiple essential functions beyond digestion. Studies demonstrate that gut bacteria protect against enteropathogens, extract nutrients and energy from dietary components, and contribute to normal immune function. [1] The microbiota produces metabolites such as short-chain fatty acids (SCFAs) that serve as signaling molecules, influencing host metabolism, immune responses, and even brain function through the gut-brain axis. [10]
Emerging evidence indicates that diverse bacterial communities provide colonization resistance against pathogenic microorganisms by consuming nutrients that pathogens require for growth. [11] This protective effect demonstrates why maintaining microbiome diversity represents a critical aspect of disease prevention.
Fermented Foods: Ancient Wisdom Meets Modern Science
Fermented foods have been integral to human diets for approximately 10,000 years, and contemporary research increasingly validates their health-promoting properties. [12] These foods undergo transformation by microorganisms, potentially delivering live beneficial bacteria, bioactive peptides, and microbial metabolites that positively influence gut microbiome composition.
Evidence-Based Benefits of Fermented Foods
A landmark clinical trial at Stanford University demonstrated that participants consuming a diet high in fermented foods for 10 weeks experienced increased gut microbiome diversity and decreased markers of inflammation. [13] The study found that eating foods such as yogurt, kefir, kimchi, and kombucha led to enhanced microbial diversity, with stronger effects observed at higher serving sizes.
Additional research reveals that fermented vegetables specifically promote production of short-chain fatty acids including acetate and propionate, which have known beneficial effects on metabolic health. [14] Regular consumers of lacto-fermented vegetables demonstrate greater diversity of fecal metabolites compared to non-consumers. [15]
Key Fermented Foods for Gut Health
Yogurt: Contains live bacterial cultures, particularly Lactobacillus and Bifidobacterium species, which may survive gastrointestinal transit and temporarily colonize the gut. [12] Look for products labeled with "live and active cultures."
Kefir: A fermented milk beverage with greater microbial diversity than yogurt, containing both bacteria and beneficial yeasts. Research suggests kefir consumption may positively influence gut microbiota composition. [16]
Kimchi and Sauerkraut: Fermented vegetables rich in lactobacilli that produce beneficial metabolites during fermentation. Studies indicate these foods can alter gut microbial communities and reduce inflammation markers. [13]
Kombucha: A fermented tea containing acetic acid bacteria and yeasts. While research is still emerging, preliminary studies suggest potential benefits for gut health and immune function. [16]
Dietary Fiber and Prebiotics: Feeding the Microbiome
Dietary fiber represents a cornerstone of gut health, serving as the primary substrate for microbial fermentation in the colon. [17] While humans lack enzymes to digest most dietary fibers, gut bacteria ferment these complex carbohydrates, producing short-chain fatty acids and other beneficial metabolites.
Understanding Short-Chain Fatty Acids
Short-chain fatty acids (SCFAs)—primarily acetate, propionate, and butyrate—represent the principal metabolites of fiber fermentation and exert multiple beneficial effects on host physiology. [18] Butyrate serves as the preferred energy source for colonocytes (intestinal epithelial cells), supporting gut barrier integrity and reducing inflammation. [19] Propionate and acetate enter systemic circulation, influencing metabolism, appetite regulation, and immune function. [20]
Research demonstrates that SCFA production varies based on fiber type, gut microbiota composition, and individual host factors. [17] While not all fiber interventions significantly increase SCFA levels in healthy adults, the beneficial effects of fiber extend beyond SCFA production alone, including improved stool consistency, transit time, and support for beneficial bacterial populations.
Prebiotic Fiber Sources
Whole Grains: Contain fermentable fibers including resistant starch and beta-glucans. Epidemiological studies associate higher whole grain intake with reduced risk of cardiovascular disease, type 2 diabetes, and colorectal cancer. [21]
Legumes: Beans, lentils, and chickpeas provide substantial amounts of fermentable fiber and resistant starch. These foods support growth of beneficial bacteria while providing essential nutrients. [21]
Chicory Root and Jerusalem Artichoke: Exceptionally rich in inulin, a prebiotic fiber that selectively stimulates growth of beneficial Bifidobacterium species. [5]
Garlic and Onions: Contain fructooligosaccharides (FOS) and inulin. Research indicates these foods may enhance populations of beneficial bacteria while providing antimicrobial compounds. [5]
Bananas: Particularly when slightly underripe, bananas provide resistant starch and fructooligosaccharides that function as prebiotics, supporting beneficial gut bacteria. [5]
Probiotics and Synbiotics: Targeted Microbiome Modulation
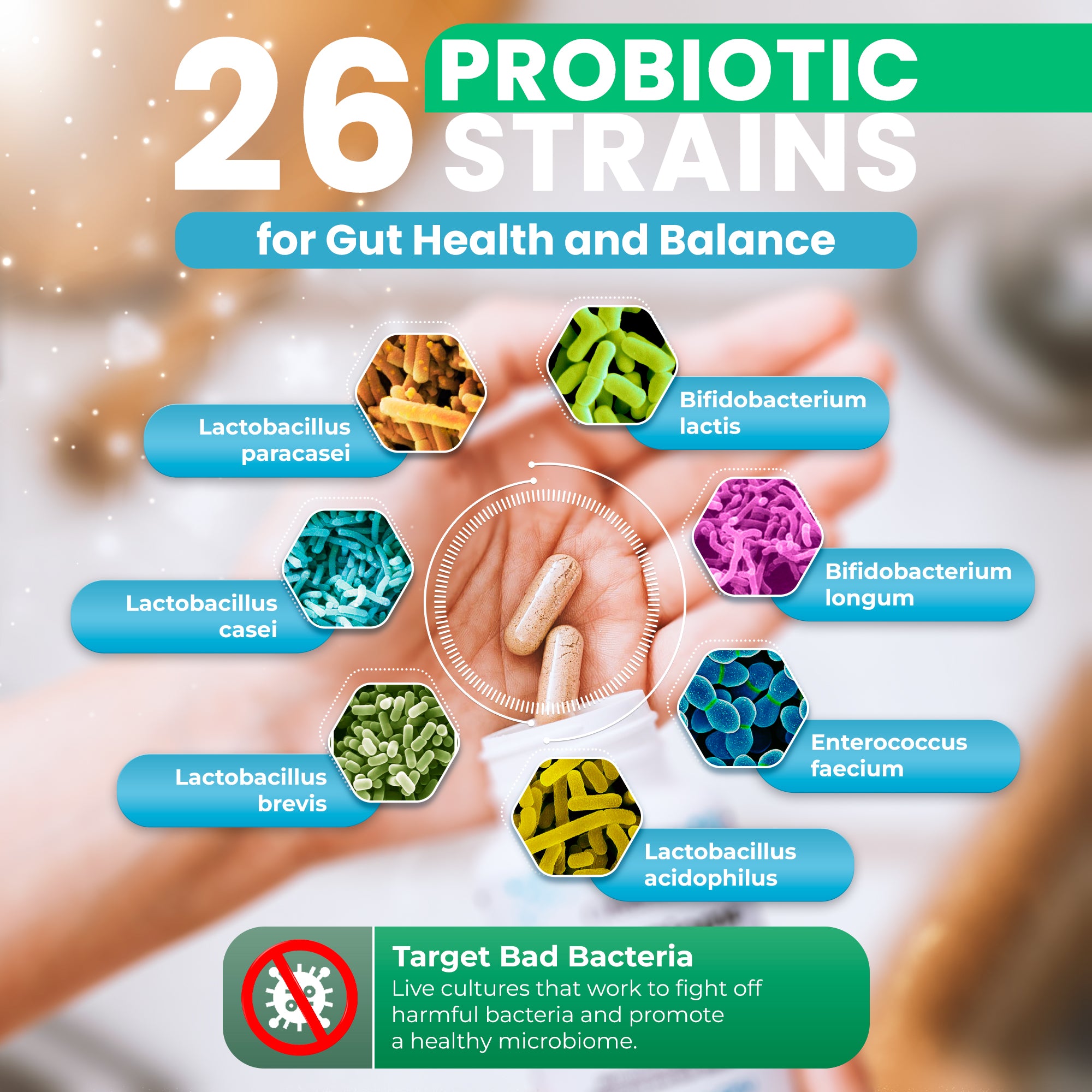
Probiotics are defined as live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. [22] Strains of Lactobacillus, Bifidobacterium, and Saccharomyces have extensive safety records and demonstrated efficacy in various clinical applications. [22]
Clinical Evidence for Probiotic Efficacy
Multiple systematic reviews and meta-analyses support probiotic use for specific conditions. Evidence is particularly strong for preventing antibiotic-associated diarrhea, reducing symptoms of irritable bowel syndrome, and supporting treatment of certain inflammatory bowel diseases. [23] However, probiotic effects are strain-specific and condition-specific, meaning benefits demonstrated for one strain cannot be assumed for another.
Recent research emphasizes that habitual diet significantly influences probiotic efficacy. [8] Clinical trials demonstrate that individuals with higher baseline fiber intake show greater microbiome responses to both prebiotic and probiotic interventions. [24] This finding underscores the importance of comprehensive dietary approaches rather than relying solely on supplementation.
Synbiotics: Combining Probiotics and Prebiotics
Synbiotics represent combinations of probiotics and prebiotics designed to work synergistically. [25] The prebiotic component provides substrate specifically utilized by the probiotic strains, potentially enhancing their survival and activity in the gut. Research on synergistic synbiotics—where components work together to produce health benefits—shows promise, though more rigorous clinical trials are needed. [5]
The Gut-Immune System Connection
Approximately 70-80% of immune cells reside in the gut, highlighting the critical importance of gut-immune interactions. [7] The gut microbiota plays essential roles in immune system development, maturation, and regulation throughout life.
Mechanisms of Immune Modulation
Research demonstrates that gut bacteria educate the immune system, helping to distinguish between harmless antigens and potential threats. [26] Germ-free animals—those raised without any microbiota—display profoundly impaired immune development, including underdeveloped gut-associated lymphoid tissue, reduced numbers of immune cells, and dysregulated immune responses. [27]
Specific bacterial species and their metabolites influence immune function through multiple mechanisms. Certain Bacteroides species produce polysaccharide A (PSA), which promotes development of regulatory T cells that help maintain immune tolerance. [26] Short-chain fatty acids, particularly butyrate, exhibit anti-inflammatory properties by inhibiting histone deacetylases and activating G-protein coupled receptors on immune cells. [28]
Implications for Disease Prevention
The gut-immune axis influences susceptibility to infections, autoimmune diseases, allergies, and even systemic conditions like cardiovascular disease. [29] Dysbiosis—imbalance in gut microbial composition—has been associated with inappropriate immune activation and chronic inflammation. [30] Conversely, maintaining diverse, balanced gut microbiota may support immune homeostasis and reduce disease risk.
Organic Approaches to Gut Health
While research specifically comparing organic versus conventional foods' effects on gut microbiota remains limited, organic agriculture may offer certain advantages for microbiome health. Studies suggest organic foods often contain higher levels of certain phytochemicals and lower pesticide residues. [31]
Enhanced Phytochemical Content
Organic produce may contain higher concentrations of beneficial plant compounds that support gut bacteria
Reduced Pesticide Exposure
Lower pesticide residues may help preserve beneficial gut bacterial populations
Sustainable Agriculture
Organic farming practices that support soil microbial diversity may translate to food quality
Nutrient Density
Some evidence suggests enhanced nutrient profiles in organically grown foods
Comprehensive Gut Health Strategies
Optimizing gut health requires a multifaceted approach incorporating dietary modifications, targeted supplementation when appropriate, and lifestyle factors including stress management, adequate sleep, and regular physical activity. [32]
Evidence-Based Recommendations for Gut Health
- Increase dietary fiber intake: Aim for 25-38 grams daily from diverse plant sources including vegetables, fruits, whole grains, and legumes [21]
- Incorporate fermented foods regularly: Include multiple servings weekly of naturally fermented foods containing live cultures [13]
- Diversify plant food consumption: Research suggests consuming 30+ different plant foods weekly promotes microbiome diversity [33]
- Limit ultra-processed foods: High consumption of processed foods associates with reduced microbiome diversity and altered metabolic function [34]
- Consider targeted probiotics: For specific conditions, evidence-based probiotic strains may provide benefits [23]
- Stay adequately hydrated: Water intake supports digestive function and nutrient absorption
- Manage stress: Chronic stress can negatively impact gut microbiota composition and barrier function [35]
- Prioritize sleep: Sleep disruption associates with altered gut microbiome composition [36]
The Role of Targeted Supplementation
While diet should form the foundation of gut health strategies, targeted supplementation with comprehensive probiotic and prebiotic formulations may support optimal microbiome function. Quality supplements should contain multiple well-researched bacterial strains, prebiotic fibers to support bacterial growth, and be free from unnecessary additives or fillers.
When considering supplementation, look for products that provide:
- Diverse strains of clinically studied probiotic bacteria
- Adequate colony-forming units (CFUs) to achieve therapeutic effects
- Prebiotic components including inulin, fructooligosaccharides, or galactooligosaccharides
- Delayed-release or enteric-coated capsules to protect bacteria through stomach acid
- Third-party testing for purity and potency
Consistency is crucial when using probiotic supplements. Research indicates that beneficial effects typically require several weeks of regular use, as the gut microbiome needs time to adjust and rebalance. [37]
Future Directions in Microbiome Research
The field of microbiome science continues to evolve rapidly. Emerging research areas include personalized nutrition based on individual microbiome profiles, identification of next-generation probiotics from novel bacterial species, and development of postbiotics—beneficial compounds produced by probiotics that may exert health effects without live bacteria. [38]
As our understanding deepens, therapeutic approaches may become increasingly sophisticated, potentially including targeted microbiome modulation for specific diseases, precision probiotic formulations based on individual gut composition, and dietary recommendations personalized to optimize individual microbiome responses. [8]
Conclusion
The gut microbiome represents a dynamic, influential component of human health that responds to dietary and lifestyle interventions. Scientific evidence strongly supports the benefits of diverse, fiber-rich diets incorporating fermented foods for maintaining optimal gut health. [4] While individual responses may vary, comprehensive approaches combining whole food nutrition, targeted supplementation when appropriate, and healthy lifestyle practices offer the most promising strategies for supporting a diverse, balanced gut microbiome.
As research continues to illuminate the complex interactions between diet, gut microbiota, and host health, these evidence-based strategies provide a solid foundation for optimizing gut health and, by extension, overall wellbeing. Supporting your gut microbiome through science-backed approaches represents an investment in long-term health across multiple physiological systems.
References
[1] Lozupone, C. A., Stombaugh, J. I., Gordon, J. I., Jansson, J. K., & Ley, R. E. (2012). Diversity, stability and resilience of the human gut microbiota. Nature, 489(7415), 220-230.
[2] Lynch, S. V., & Pedersen, O. (2016). The Human Intestinal Microbiome in Health and Disease. New England Journal of Medicine, 375(24), 2369-2379.
[3] Le Chatelier, E., Nielsen, T., Qin, J., et al. (2013). Richness of human gut microbiome correlates with metabolic markers. Nature, 500(7464), 541-546.
[4] David, L. A., Maurice, C. F., Carmody, R. N., et al. (2014). Diet rapidly and reproducibly alters the human gut microbiome. Nature, 505(7484), 559-563.
[5] Whelan, K., Alexander, M., Gaiani, C., et al. (2024). Design and reporting of prebiotic and probiotic clinical trials in the context of diet and the gut microbiome. Nature Microbiology, 9(11), 2785-2794.
[6] Parada Venegas, D., De la Fuente, M. K., Landskron, G., et al. (2019). Short-chain fatty acids (SCFAs)-mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases. Frontiers in Immunology, 10, 277.
[7] Wiertsema, S. P., van Bergenhenegouwen, J., Garssen, J., & Knippels, L. M. J. (2021). The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients, 13(3), 886.
[8] Wastyk, H. C., et al. (2023). Randomized controlled trial demonstrates response to a probiotic intervention for metabolic syndrome that may correspond to diet. Gut Microbes, 15(1), 2178794.
[9] Yatsunenko, T., Rey, F. E., Manary, M. J., et al. (2012). Human gut microbiome viewed across age and geography. Nature, 486(7222), 222-227.
[10] Silva, Y. P., Bernardi, A., & Frozza, R. L. (2020). The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Frontiers in Endocrinology, 11, 25.
[11] Spragge, F., Bakkeren, E., Jahn, M. T., et al. (2023). Microbiome diversity protects against pathogens by nutrient blocking. Science, 382(6676), eadj3502.
[12] Melini, F., Melini, V., Luziatelli, F., Ficca, A. G., & Ruzzi, M. (2019). Fermented Foods, Health and the Gut Microbiome. Nutrients, 11(8), 1806.
[13] Wastyk, H. C., Fragiadakis, G. K., Perelman, D., et al. (2021). Gut-microbiota-targeted diets modulate human immune status. Cell, 184(16), 4137-4153.e14.
[14] Chambers, E. S., Preston, T., Frost, G., & Morrison, D. J. (2018). Role of Gut Microbiota-Generated Short-Chain Fatty Acids in Metabolic and Cardiovascular Health. Current Nutrition Reports, 7(4), 198-206.
[15] Guse, K., Trojan, A., Sahadew, S., et al. (2023). Fermented vegetables positively impact gut health. Gut Microbiomes, 4, e6.
[16] Dimidi, E., Cox, S. R., Rossi, M., & Whelan, K. (2019). Fermented foods: definitions and characteristics, impact on the gut microbiota and effects on gastrointestinal health and disease. Nutrients, 11(8), 1806.
[17] Barber, T. M., Kabisch, S., Pfeiffer, A. F. H., & Weickert, M. O. (2020). The Health Benefits of Dietary Fibre. Nutrients, 12(10), 3209.
[18] den Besten, G., van Eunen, K., Groen, A. K., Venema, K., Reijngoud, D. J., & Bakker, B. M. (2013). The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. Journal of Lipid Research, 54(9), 2325-2340.
[19] Liu, H., Wang, J., He, T., et al. (2018). Butyrate: A Double-Edged Sword for Health? Advances in Nutrition, 9(1), 21-29.
[20] Frost, G., Sleeth, M. L., Sahuri-Arisoylu, M., et al. (2014). The short-chain fatty acid acetate reduces appetite via a central homeostatic mechanism. Nature Communications, 5, 3611.
[21] Reynolds, A., Mann, J., Cummings, J., Winter, N., Mete, E., & Te Morenga, L. (2019). Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. The Lancet, 393(10170), 434-445.
[22] Sanders, M. E., Merenstein, D. J., Reid, G., Gibson, G. R., & Rastall, R. A. (2019). Probiotics and prebiotics in intestinal health and disease: from biology to the clinic. Nature Reviews Gastroenterology & Hepatology, 16(10), 605-616.
[23] Yassine, F., Najm, A., & Bilen, M. (2025). The role of probiotics, prebiotics, and synbiotics in the treatment of inflammatory bowel diseases: an overview of recent clinical trials. Frontiers in Systems Biology, 5, 1561047.
[24] Healey, G., Murphy, R., Butts, C., et al. (2018). Habitual dietary fibre intake influences gut microbiota response to an inulin-type fructan prebiotic: a randomised, double-blind, placebo-controlled, cross-over, human intervention study. British Journal of Nutrition, 119(2), 176-189.
[25] Swanson, K. S., Gibson, G. R., Hutkins, R., et al. (2020). The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of synbiotics. Nature Reviews Gastroenterology & Hepatology, 17(11), 687-701.
[26] Wu, H. J., & Wu, E. (2012). The role of gut microbiota in immune homeostasis and autoimmunity. Gut Microbes, 3(4), 4-14.
[27] Gensollen, T., Iyer, S. S., Kasper, D. L., & Blumberg, R. S. (2016). How colonization by microbiota in early life shapes the immune system. Science, 352(6285), 539-544.
[28] Kim, C. H. (2021). Control of lymphocyte functions by gut microbiota-derived short-chain fatty acids. Cellular & Molecular Immunology, 18(5), 1161-1171.
[29] Zheng, D., Liwinski, T., & Elinav, E. (2020). Interaction between microbiota and immunity in health and disease. Cell Research, 30(6), 492-506.
[30] Shi, N., Li, N., Duan, X., & Niu, H. (2017). Interaction between the gut microbiome and mucosal immune system. Military Medical Research, 4, 14.
[31] Hurtado-Barroso, S., Tresserra-Rimbau, A., Vallverdú-Queralt, A., & Lamuela-Raventós, R. M. (2019). Organic food and the impact on human health. Critical Reviews in Food Science and Nutrition, 59(4), 704-714.
[32] Mayer, E. A., Nance, K., & Chen, S. (2022). The Gut-Brain Axis. Annual Review of Medicine, 73, 439-453.
[33] McDonald, D., Hyde, E., Debelius, J. W., et al. (2018). American Gut: an Open Platform for Citizen Science Microbiome Research. mSystems, 3(3), e00031-18.
[34] Zinöcker, M. K., & Lindseth, I. A. (2018). The Western Diet-Microbiome-Host Interaction and Its Role in Metabolic Disease. Nutrients, 10(3), 365.
[35] Madison, A., & Kiecolt-Glaser, J. K. (2019). Stress, depression, diet, and the gut microbiota: human-bacteria interactions at the core of psychoneuroimmunology and nutrition. Current Opinion in Behavioral Sciences, 28, 105-110.
[36] Smith, R. P., Easson, C., Lyle, S. M., et al. (2019). Gut microbiome diversity is associated with sleep physiology in humans. PLoS ONE, 14(10), e0222394.
[37] Suez, J., Zmora, N., Segal, E., & Elinav, E. (2019). The pros, cons, and many unknowns of probiotics. Nature Medicine, 25(5), 716-729.
[38] Salminen, S., Collado, M. C., Endo, A., et al. (2021). The International Scientific Association of Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics. Nature Reviews Gastroenterology & Hepatology, 18(9), 649-667.







Share and get 15% off!
Simply share this product on one of the following social networks and you will unlock 15% off!