Sugar cravings can be hard to deal with, even for people who try to eat healthy. But what if the answer to controlling them is in your gut? Recent scientific breakthroughs reveal that specific gut bacteria literally control your desire for sweets through a sophisticated communication system between your digestive tract and brain. Scientists discovered that mice missing certain gut bacteria consumed 50% more sugar than healthy mice—and this preference reversed when beneficial bacteria were restored [1]. Let's explore how probiotics and prebiotics might help reduce your desire for sweets and fundamentally change how you manage your sugar intake.
| Key Takeaways |
|---|
| • Specific gut bacteria like Bacteroides vulgatus produce compounds that naturally suppress sugar cravings through the gut-brain axis • Clinical trials show certain probiotic strains reduce sugar consumption by 19% and food cravings by 91% • Your gut produces 50% of your body's dopamine and 95% of its serotonin—neurotransmitters that control cravings • Probiotics work like natural GLP-1 (similar to Ozempic) by producing short-chain fatty acids that increase satiety • Combining probiotics with prebiotics creates synergistic effects for better craving control • Stress and poor sleep disrupt gut bacteria, intensifying sugar cravings through inflammatory pathways |
Understanding the Gut-Brain Axis: Your Internal Communication Highway
Your gut and brain maintain constant communication through what scientists call the gut-brain axis—a sophisticated biological network that profoundly influences what you want to eat. The gut microbiome, consisting of trillions of microorganisms living in your digestive tract, plays a commanding role in this conversation, affecting not just digestion but also your mood, metabolism, and food choices [2].
The vagus nerve serves as the primary communication highway in this system, acting like a fiber optic cable transmitting signals between your gut and brain. Remarkably, 80% of these nerve signals travel upward from gut to brain, carrying information about gut hormones, bacterial metabolites, and satiety signals to appetite-regulating centers in your hypothalamus [3]. This constant stream of data from your gut microbiota shapes your food preferences in real-time.
Some bacteria in your gut thrive on sugar and simple carbohydrates. When there are too many of these sugar-loving microbes, they send signals that intensify your cravings for sweet foods—essentially voting for their own survival. Research shows that people with lower gut microbiome diversity tend to have stronger cravings and consume more sugar [4]. On the other hand, when you maintain a balanced gut microbiota composition with plenty of beneficial bacteria, you experience greater satisfaction from meals and fewer intense cravings.
A groundbreaking 2025 study in Nature Microbiology revealed exactly how this works: Bacteroides vulgatus, a beneficial gut bacterium, produces pantothenate (vitamin B5), which triggers a cascade that promotes GLP-1 secretion. This hormone then inhibits sugar preference by stimulating hepatic FGF21 release—creating a complete gut microbiota-metabolite-hormone-brain axis that controls dietary choice [1]. Diabetic patients have significantly lower levels of B. vulgatus, and supplementation with this bacterium or pantothenate reduced sugar preference and improved metabolic parameters in both mice and humans.
This is where probiotics and prebiotics become crucial tools. They can help rebalance your gut microbiota, potentially changing not just how you digest food but fundamentally altering your relationship with sugar.
What Are Probiotics and Prebiotics?
Probiotics are live beneficial bacteria that support your health when consumed in adequate amounts. They primarily colonize your gut, where they help with digestion, protect your intestinal barrier, support immune system function, and produce essential neurotransmitters. You can find probiotics in fermented foods like yogurt, kefir, sauerkraut, and kimchi, as well as in targeted probiotic supplements.
The World Health Organization defines probiotics as "live microorganisms which, when administered in adequate amounts, confer a health benefit on the host." Clinical trials typically use doses ranging from 1-20 billion colony-forming units (CFU) daily, though metabolic benefits generally require at least 10 billion CFU [5].
Prebiotics are specialized types of fiber that your body cannot digest but your gut bacteria can ferment. They essentially serve as food for beneficial bacteria, helping them flourish and produce health-promoting compounds. Foods rich in prebiotics include onions, garlic, bananas, asparagus, oats, and Jerusalem artichokes. Eating a variety of prebiotic foods helps cultivate and sustain populations of good bacteria in your gut, leading to a healthier, more diverse gut microbiota overall.
When you combine probiotics with prebiotics, you create what scientists call a synbiotic—a powerful partnership that enhances gut health more effectively than either component alone. This combination ensures that beneficial bacteria have both the initial population boost (from probiotics) and the sustained nourishment (from prebiotics) they need to thrive long-term.
The Neuroscience of Sugar Addiction: Why Cravings Feel Irresistible
Sugar addiction isn't about willpower—it's neuroscience. Research demonstrates that sugar activates the same dopamine reward pathways in your brain as cocaine, and brain imaging studies show that people with obesity have reduced dopamine D2 receptor availability similar to those with substance use disorders [6]. This neurological similarity helps explain why sugar cravings can feel genuinely compulsive.
Scientists recently discovered that your gut contains separate populations of vagal neurons that detect sugar versus fat, and these distinct signals travel to different dopaminergic circuits in your brain's ventral tegmental area (the reward center). When you consume foods containing both sugar and fat together—like ice cream, cookies, or chocolate—both pathways activate simultaneously, producing a multiplicative dopamine release that's 2-3 times greater than either nutrient alone [7]. This synergistic effect explains why ultra-processed foods engineered with sugar-fat combinations are so difficult to resist.
Your gut bacteria directly influence these reward circuits. Approximately 50% of your body's dopamine and 95% of its serotonin are produced in your gut by specific bacterial strains and intestinal cells [8]. Certain Bacillus and Escherichia strains produce dopamine from L-DOPA, while Lactobacilli and Bifidobacteria convert glutamate to GABA—a calming neurotransmitter that reduces anxiety-driven eating. When gut dysbiosis occurs (an imbalance favoring harmful bacteria), the production of these crucial neurotransmitters declines, making you more vulnerable to intense cravings and compulsive eating behaviors.
Food addiction represents a genuine clinical condition. Studies using the Yale Food Addiction Scale reveal that approximately 33% of people who've undergone bariatric surgery meet diagnostic criteria for food addiction, characterized by loss of control, continued use despite consequences, and tolerance requiring increased amounts for satisfaction [9]. Emerging research shows that binge eating disorder and food addiction are strongly associated with distinct gut microbiota profiles, with patients showing lower levels of beneficial bacteria like Akkermansia and altered short-chain fatty acid production [10].
The encouraging news: probiotics can help restore healthy neurotransmitter production and normalize reward circuit function. Clinical trials demonstrate that specific probiotic interventions significantly reduce both food addiction scores and binge eating behaviors, with effects persisting at one-year follow-up [11].
How Probiotics Reduce Sugar Cravings: Five Powerful Mechanisms
Probiotics employ multiple sophisticated strategies to help control sugar cravings:
1. Improving Blood Sugar Regulation
Specific probiotic strains improve how your body processes insulin and handles glucose, leading to more stable blood sugar levels throughout the day. A meta-analysis of 15 animal studies found that Akkermansia muciniphila administration significantly reduced fasting blood glucose by 21.2% [12]. When blood sugar remains stable rather than spiking and crashing, you experience fewer sudden, intense cravings for quick-energy foods like sweets. This steadier metabolic state helps break the cycle of sugar-induced blood sugar fluctuations that perpetuate cravings.
2. Increasing Satiety Through Hormone Modulation
Certain probiotics influence the production of hormones that control hunger and fullness, particularly GLP-1 (glucagon-like peptide-1) and PYY (peptide YY). When beneficial gut bacteria ferment dietary fiber, they produce short-chain fatty acids (SCFAs)—primarily acetate, propionate, and butyrate. These SCFAs bind to receptors called FFAR2 and FFAR3 on specialized intestinal L-cells, stimulating them to release GLP-1 and PYY [13].
GLP-1 is particularly significant because it's the same appetite-suppressing hormone mimicked by popular weight loss medications like Ozempic and Wegovy. However, probiotics stimulate your body to produce GLP-1 naturally, without injections or pharmaceutical side effects. Clinical studies show that probiotic supplementation can increase GLP-1 levels by up to 40%, providing substantial appetite control [14].
Akkermansia muciniphila produces proteins that directly stimulate GLP-1 release from intestinal cells. In human trials, 91% of participants taking Akkermansia experienced fewer overall food cravings, and 86% specifically noted reduced sugar cravings over 3 months [12]. These SCFAs also cross the blood-brain barrier and directly affect appetite-regulating neurons in your hypothalamus, further enhancing satiety signals.
3. Modifying Brain Response to Sweet Tastes
Probiotics can alter how your brain's reward centers respond to sweet flavors, potentially making sugary foods less appealing over time. This occurs through multiple pathways: by increasing dopamine and serotonin production in the gut (which then influences brain levels), by reducing inflammatory signaling that disrupts reward circuits, and by modulating the gut-brain communication that shapes taste preferences [2].
Research with specific Lactobacillus strains showed they reduced stress-induced sugar consumption by 19% within just 27 days by modulating dopamine and serotonin levels in brain regions controlling appetite, reward, and mood [15]. While we need more human research to fully understand these mechanisms, many people report experiencing decreased desire for sweets after several weeks of consistent probiotic supplementation.
4. Producing Appetite-Regulating Metabolites
Beyond SCFAs, gut bacteria produce numerous other metabolites that influence appetite and cravings. Tryptophan metabolism by beneficial bacteria produces indole derivatives that stimulate serotonin production, improving mood and reducing emotional eating [16]. Some bacterial proteins, like ClpB produced by Enterobacteriaceae, can act as mimics of appetite-suppressing hormones like α-MSH, directly activating satiety receptors and enhancing the release of fullness hormones [16].
The bacterial metabolite pantothenate (vitamin B5), produced by Bacteroides vulgatus, has emerged as a key regulator of sugar preference. This compound promotes GLP-1 secretion, which then stimulates the liver to release FGF21—a hormone that suppresses sweet taste preference and reduces sugar intake [1]. Supplementation studies show this pathway can reduce sugar consumption while improving overall metabolic health markers.
5. Reducing Inflammation That Drives Cravings
Chronic low-grade inflammation significantly amplifies food cravings. Studies reveal that people with stronger cravings have 2-3 times higher levels of inflammatory cytokines, particularly IL-6 and IL-8, with correlation coefficients ranging from 0.312-0.340 [17]. These inflammatory molecules cross the blood-brain barrier and interfere with normal neurotransmitter production, particularly serotonin and dopamine, which regulate mood and reward processing.
Beneficial probiotics produce anti-inflammatory compounds and strengthen the intestinal barrier, preventing inflammatory molecules from entering circulation. A Stanford study found that a 10-week diet rich in fermented foods (which naturally contain probiotics) decreased 19 different inflammatory markers and increased gut microbiome diversity in a dose-dependent manner—those consuming the most fermented foods experienced the greatest reduction in inflammation [18].
Probiotic Strains Scientifically Proven to Reduce Sugar Cravings
Not all probiotics offer equal benefits for managing sugar cravings. Research has identified specific strains with demonstrated efficacy:
Lactobacillus gasseri BNR17
This strain has robust clinical evidence for metabolic health and weight management. A 12-week randomized controlled trial with 90 adults (BMI 25-35) found that high-dose L. gasseri BNR17 (10 billion CFU daily) significantly decreased visceral adipose tissue, body fat mass, and percent body fat compared to placebo [19]. Animal studies reveal it works by increasing fatty acid oxidation genes while decreasing fatty acid synthesis genes, along with reducing leptin and insulin levels.
A separate study in mice fed a high-sucrose diet showed that L. gasseri BNR17 prevented weight gain and fat accumulation specifically caused by excess sugar consumption [20]. This strain is particularly valuable because it's available in some Greek yogurt brands and targeted supplements, making it accessible for daily use.
Lactobacillus salivarius + Lactobacillus gasseri Combination
This represents the first published study demonstrating direct sugar craving reduction in a controlled setting. Researchers supplemented stressed mice with L. salivarius LS7892 and L. gasseri LG6410, which reduced sucrose intake by 19% during chronic stress exposure [15]. The strains modulated dopamine and serotonin levels in brain regions controlling appetite and mood, effectively reducing stress-induced hyperphagia (overeating). This combination specifically targets stress-related sugar consumption—a common pattern for many people.
Bacteroides vulgatus
This bacterium produces pantothenate (vitamin B5), which promotes GLP-1 secretion that inhibits sugar preference through hepatic FGF21 release. The abundance of B. vulgatus negatively correlates with sugar intake in both mice and humans, and levels are significantly lower in diabetic patients [1]. Supplementation with either B. vulgatus itself or pantothenate reduced sugar preference while improving metabolic parameters including glucose tolerance and insulin sensitivity. This represents a complete, mechanistically-defined pathway from gut bacteria to reduced sugar cravings.
Akkermansia muciniphila
This mucin-degrading bacterium has generated substantial excitement in metabolic health research. A meta-analysis of 15 animal studies showed Akkermansia administration reduced body weight gain by 10.4% and fasting blood glucose by 21.2% [12]. In human trials, 91% of participants experienced fewer food cravings overall, and 86% noted reduced sugar cravings specifically over 3 months.
Akkermansia works through multiple mechanisms: it strengthens the intestinal barrier (reducing inflammatory signaling), increases production of short-chain fatty acids (particularly butyrate), and produces proteins that directly stimulate GLP-1 secretion from intestinal cells [21]. A human clinical trial published in Cell Metabolism found that Akkermansia supplementation in overweight/obese adults with type 2 diabetes significantly reduced body weight, fat mass, and HbA1c—but only in participants who had low baseline levels of the bacterium [22]. This suggests testing baseline levels may help predict who will benefit most from supplementation.
Bifidobacterium breve B-3
A 12-week randomized controlled trial with 80 pre-obese adults (BMI 25-30) showed that B. breve B-3 supplementation (20 billion CFU daily) prevented increases in visceral fat area during the study period, while the placebo group experienced fat accumulation [23]. Body fat mass and body fat percentage were significantly lower in the B-3 group at weeks 8 and 12. This strain appears to offer specific benefits for preventing weight gain and fat accumulation, which often accompanies habitual sugar consumption.
Multi-Strain Combinations for Eating Disorders
Clinical research on food addiction and binge eating has primarily used multi-strain formulations. A landmark randomized controlled trial with 101 post-bariatric surgery patients used a combination of Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07 (5 billion CFU each) for 90 days [11]. At one-year follow-up, the probiotic group showed significantly lower Yale Food Addiction Scale symptoms (p=0.037) and Binge Eating Scale scores (p=0.030) compared to placebo, with 99% adherence. The researchers proposed the benefits occurred through multiple mechanisms: modulation of the microbiota-gut-brain axis, increased SCFA production, reduced inflammation, downregulation of the stress-responsive HPA axis, and improved biosynthesis of serotonin and GABA.
The Power of Prebiotics: Feeding Your Beneficial Bacteria
Prebiotics are equally important as probiotics for managing sugar cravings and optimizing gut health. These specialized fibers selectively feed beneficial bacteria, helping them proliferate and function optimally. By nourishing helpful microbes, prebiotics create an intestinal environment that favors beneficial bacteria while discouraging harmful species.
Inulin represents one of the most studied prebiotics, found abundantly in Jerusalem artichokes, chicory root, onions, and garlic. Inulin can help stabilize blood sugar levels by slowing how your body digests and absorbs carbohydrates, leading to fewer sudden spikes and crashes that trigger sugar cravings [24]. Inulin specifically promotes the growth of beneficial bacteria like Bifidobacteria and Lactobacilli, which are associated with better metabolic health, reduced inflammation, and potentially fewer sugar cravings.
Other important prebiotic fibers include:
- Fructooligosaccharides (FOS): Found in onions, garlic, bananas, and asparagus. FOS selectively stimulates Bifidobacterium growth and increases SCFA production.
- Galactooligosaccharides (GOS): Present in legumes and human milk. GOS promotes beneficial Bifidobacteria and Lactobacilli while inhibiting pathogenic bacteria.
- Resistant starch: Found in slightly underripe bananas, cooked and cooled potatoes and rice, and legumes. Resistant starch fermentation produces substantial amounts of butyrate, the SCFA most strongly associated with metabolic health.
- Beta-glucan: Abundant in oats and barley. This soluble fiber forms a gel in your digestive tract, slowing glucose absorption while feeding beneficial bacteria.
- Pectin: Found in apples, citrus fruits, and berries. Pectin serves as food for SCFA-producing bacteria and has additional benefits for blood sugar control.
The key is variety. Different prebiotics support different beneficial bacteria, so consuming a diverse array of prebiotic foods helps maintain a robust, diverse gut microbiome. Start gradually if you're not accustomed to high-fiber foods, as sudden increases can cause temporary digestive discomfort like gas and bloating. Most people adapt within 1-2 weeks as their gut bacteria adjust.
Choosing the right prebiotics can make a significant difference in your gut health and sugar craving management.
The Dynamic Duo: Synbiotics for Superior Results
When you deliberately combine probiotics and prebiotics, you create a synbiotic—a formulation designed to maximize the survival, colonization, and activity of beneficial bacteria in your gut. The scientific rationale is compelling: providing both the beneficial bacteria (probiotics) and their preferred food source (prebiotics) substantially improves the probiotics' ability to survive stomach acid, colonize your intestines, and produce beneficial metabolites.
A healthy gut microbiome supported by synbiotics translates to fewer sugar cravings and better food choices overall. Think of it as recruiting a team of microscopic helpers for your digestive system, all working synergistically to keep you feeling satisfied and less likely to reach for sugary snacks. This combination creates a more stable and diverse gut ecosystem, which research consistently links to improved digestion, enhanced nutrient absorption, stronger intestinal barrier function, and better regulation of appetite hormones.
Practical synbiotic combinations you can implement immediately:
- Greek yogurt with berries and ground flaxseed: Provides Lactobacillus and Bifidobacterium strains (probiotics) along with pectin from berries and fiber from flaxseed (prebiotics)
- Kefir blended with banana and oats: Delivers 30-60 diverse bacterial strains (probiotics) plus resistant starch from banana and beta-glucan from oats (prebiotics)
- Sauerkraut with a side of roasted Jerusalem artichokes: Combines Lactobacillus-rich fermented cabbage (probiotic) with inulin-rich Jerusalem artichokes (prebiotic)
- Kimchi added to a meal containing onions and garlic: Pairs diverse fermented vegetable bacteria (probiotics) with FOS-rich alliums (prebiotics)
You can also find commercial synbiotic supplements that combine specific probiotic strains with complementary prebiotics in scientifically-validated ratios.
Natural Sources of Prebiotics: Building Your Fiber Foundation
You can obtain prebiotics from many common, affordable foods. Incorporating these regularly provides sustained nourishment for your beneficial gut bacteria:
- Onions and garlic: Rich in inulin and fructooligosaccharides (FOS). Both raw and cooked forms provide prebiotic benefits, though some compounds are more concentrated when raw. Add them generously to soups, stir-fries, salads, and sauces.
- Bananas: Contain resistant starch, especially when slightly underripe. As bananas ripen, resistant starch converts to regular starch, so greener bananas offer more prebiotic benefit. They're also rich in FOS.
- Asparagus: High in inulin. Just 5 medium spears provide approximately 2 grams of prebiotic fiber. Asparagus also contains other beneficial compounds that support liver detoxification.
- Oats: Contain beta-glucan, a powerful prebiotic fiber that forms a beneficial gel in your digestive tract. Steel-cut oats and rolled oats both work well. Overnight oats allow some fermentation to begin, potentially increasing benefits.
- Jerusalem artichokes (sunchokes): One of the richest sources of inulin, containing up to 31% inulin by weight. Start with small amounts as they can cause gas in those unaccustomed to them.
- Chicory root: Often used as a coffee substitute, chicory is exceptionally high in inulin (approximately 68% of fiber content). You can find chicory root fiber added to some high-fiber foods and supplements.
- Leeks: Another excellent source of inulin and FOS. Use both the white and light green parts in soups, quiches, or sautéed as a side dish.
- Apples: Rich in pectin, a type of soluble fiber with prebiotic effects. The pectin is concentrated in the skin, so eat apples unpeeled when possible.
- Legumes: Beans, lentils, and chickpeas provide substantial amounts of resistant starch and other prebiotic fibers, plus they're excellent protein sources.
Eating a variety of these foods helps feed diverse populations of good gut bacteria, promoting a more balanced microbiome that may reduce sugar cravings. It's important to increase prebiotic-rich foods gradually to allow your gut bacteria and digestive system to adapt, especially if you're currently eating a low-fiber diet. Most experts recommend aiming for 25-35 grams of total fiber daily, with at least 5-10 grams coming from prebiotic sources.
The Role of Gut Health in Blood Sugar Control
Your gut microbiome affects far more than just cravings—it fundamentally influences how your body manages glucose and maintains stable blood sugar levels. A balanced gut microbiota contributes to blood sugar regulation through several sophisticated mechanisms:
First, specific gut bacteria ferment dietary fiber into short-chain fatty acids (SCFAs), particularly acetate, propionate, and butyrate. These SCFAs improve insulin sensitivity—meaning your cells respond more effectively to insulin's signal to absorb glucose from the bloodstream. Butyrate, in particular, serves as the primary energy source for colonocytes (cells lining your colon) and has been shown to enhance glucose metabolism and insulin sensitivity throughout the body [25]. This leads to more stable blood sugar levels and fewer dramatic drops in glucose that trigger intense cravings for quick-energy sweets.
Second, a healthy gut microbiome helps maintain the integrity of your intestinal barrier—the selective filter that determines what passes from your gut into your bloodstream. When this barrier becomes compromised (often called "leaky gut"), bacterial fragments and inflammatory molecules can enter circulation, triggering systemic inflammation and insulin resistance [26]. Both inflammation and insulin resistance disrupt normal blood sugar control and can intensify cravings for sugary foods as your cells struggle to efficiently use available glucose.
Third, beneficial gut bacteria influence the production and activity of incretin hormones, particularly GLP-1 and GIP (glucose-dependent insulinotropic polypeptide). These hormones stimulate insulin secretion in response to meals, slow gastric emptying (keeping you fuller longer), and directly suppress appetite. The SCFA propionate has been shown to stimulate GLP-1 secretion, creating a direct link between gut bacteria metabolism and blood sugar control [27].
When your blood sugar remains stable rather than experiencing peaks and valleys, you're far less likely to experience sudden drops in glucose that trigger intense cravings for immediate energy from sugary snacks. This represents another crucial pathway through which probiotics and prebiotics help curb sugar cravings—by fostering a gut environment that supports balanced, steady blood sugar levels throughout the day.
Understanding how probiotics affect your gut can help you make informed choices about your health and potentially lead to better blood sugar control and reduced sugar cravings.
Stress, Gut Health, and Sugar Cravings: Breaking the Vicious Cycle
Stress profoundly impacts your gut health and dramatically amplifies sugar cravings through multiple interconnected pathways. When you experience stress, your body releases cortisol and other stress hormones. Elevated cortisol increases appetite generally but particularly drives cravings for high-calorie, sugary foods as your body seeks quick energy to cope with perceived threats [28].
Chronic stress directly alters the composition and function of your gut microbiota, potentially reducing beneficial bacteria by up to 60% while allowing harmful species to proliferate [29]. This stress-induced gut dysbiosis creates a destructive cycle: stress leads to increased sugar consumption, which feeds sugar-loving bacteria, which further disrupts the microbiome, which intensifies both stress responses and cravings. This cycle becomes self-perpetuating without intervention.
The stress-gut-cravings triangle operates through several mechanisms:
Inflammatory pathway: Chronic stress increases intestinal permeability ("leaky gut"), allowing bacterial fragments to enter circulation and trigger systemic inflammation. These inflammatory cytokines (IL-6, IL-8, TNF-α) travel to the brain, where they interfere with normal dopamine and serotonin production—the neurotransmitters that regulate mood, reward processing, and cravings [17]. Studies show people with higher inflammatory markers have significantly stronger sugar cravings.
HPA axis dysregulation: The hypothalamic-pituitary-adrenal axis becomes overactive during chronic stress, continuously releasing cortisol. This disrupts the normal circadian rhythms of your gut bacteria, reduces SCFA production, and alters neurotransmitter synthesis—all factors that influence cravings and eating behavior.
Neurotransmitter depletion: Chronic stress depletes tryptophan, the amino acid precursor to serotonin, as the body redirects it toward stress response pathways. Since 95% of serotonin is produced in the gut with the help of beneficial bacteria, stress-induced gut dysbiosis further compromises serotonin production, leading to low mood and increased emotional eating [8].
Probiotics and prebiotics offer several mechanisms to mitigate stress-related cravings:
- Some probiotic strains, particularly Lactobacillus and Bifidobacterium species, have demonstrated the ability to lower cortisol levels and reduce other stress biomarkers in both animal and human studies [29]. These are sometimes called "psychobiotics" due to their mood-regulating effects.
- Beneficial bacteria produce neurotransmitters like serotonin, dopamine, and GABA that help regulate mood and the stress response. Approximately 50% of dopamine and 95% of serotonin in your body originates in your gut [8]. Maintaining healthy populations of these neurotransmitter-producing bacteria through probiotic supplementation supports better stress resilience.
- A robust gut microbiome strengthened by probiotics and prebiotics helps maintain the intestinal barrier, reducing stress-induced intestinal permeability and preventing the cascade of inflammatory signaling that amplifies cravings.
A groundbreaking 4-week randomized controlled trial demonstrated that a diet rich in fermented foods (a "psychobiotic diet") reduced perceived stress by 32% compared to 17% in controls, lowered cortisol levels, and improved sleep quality [30]. The participants consuming the most fermented foods experienced the greatest benefits, showing a dose-response relationship.
By promoting a more balanced gut environment, probiotics and prebiotics help your body manage stress more effectively, potentially leading to fewer stress-related sugar cravings. It's like cultivating inner calm that radiates from your gut to your mind, fostering a healthier relationship between your microbiome, brain, and food choices.
Sleep and Its Impact on Cravings
Quality sleep is essential for maintaining gut health and managing sugar cravings, yet this connection is often overlooked. Poor sleep disrupts the delicate balance of your gut microbiota, which can lead to increased cravings for sugary and high-calorie foods [31]. This relationship is bidirectional—while inadequate sleep negatively impacts your gut microbiome, an imbalanced gut can also make it harder to achieve restorative sleep.
Sleep deprivation affects gut health through several pathways:
- It rapidly alters both the diversity and composition of gut bacteria, with measurable changes occurring after just a few nights of poor sleep. Studies show that sleep-restricted individuals develop gut microbiota profiles similar to those seen in obesity and metabolic syndrome.
- It increases systemic inflammation throughout the body, including in the gut, which damages the intestinal barrier and disrupts normal bacterial populations.
- It dysregulates the production of appetite-controlling hormones, particularly ghrelin (which stimulates hunger) and leptin (which signals fullness). Sleep-deprived individuals show elevated ghrelin and reduced leptin, creating a hormonal environment that drives overconsumption—particularly of sugary, high-carbohydrate foods that provide quick energy [32]. Research shows sleep-deprived people consume up to 50% more sugary foods than well-rested individuals.
Your gut microbiome, in turn, significantly influences sleep quality. Remarkably, approximately 90% of the body's serotonin—a precursor to the sleep hormone melatonin—is produced in the gut by enterochromaffin cells with the assistance of beneficial bacteria [8]. When gut dysbiosis occurs, serotonin and melatonin production declines, disrupting your natural sleep-wake cycle (circadian rhythm) and making it difficult to fall asleep or maintain deep sleep.
Emerging research suggests probiotics may improve sleep quality through several mechanisms:
- Certain probiotic strains, particularly Lactobacillus and Bifidobacterium species, influence the production of neurotransmitters like serotonin and melatonin that are crucial for regulating sleep-wake cycles [31]. By supporting healthy gut populations of these bacteria, you can enhance your body's natural production of sleep-promoting compounds.
- A healthier gut microbiome fostered by probiotics may help reduce inflammation and modulate stress hormone production, both of which can interfere with restorative sleep when elevated.
- Probiotics can alleviate digestive issues such as acid reflux, bloating, and discomfort that commonly disrupt sleep, allowing for more restful nights.
Improved sleep quality, in turn, reduces cravings and supports better gut health overall, creating a positive reinforcing cycle. By focusing on both sleep hygiene practices and gut health through strategic use of probiotics and prebiotics, you can address two interconnected factors that powerfully influence sugar cravings and support overall well-being.
Choosing the Right Probiotic and Prebiotic Combination
Not all probiotics and prebiotics offer equivalent benefits, and different strains and fiber types can produce distinct effects on your body and sugar cravings. When selecting a probiotic and prebiotic supplement or planning your dietary approach, consider these evidence-based factors:
- Bacterial strain specificity: Different strains of probiotics have different effects, even within the same species. For example, Lactobacillus gasseri BNR17 has strong clinical evidence for reducing visceral fat and improving metabolic health, while other L. gasseri strains may not share these exact properties. Look for products that specify strain designations (the letters and numbers after the species name) and cite supporting research. For managing sugar cravings and metabolic health, prioritize strains from the Lactobacillus, Bifidobacterium, Akkermansia, and Bacteroides genera that have published clinical data. The appetite-regulating mechanisms behind sugar cravings overlap significantly with the pathways involved in visceral fat storage — for the clinical evidence on specific strains that address both, see our guide to the best probiotics for belly fat.
- Prebiotic diversity: Seek supplements or dietary patterns that include a variety of prebiotic fibers—such as inulin, FOS (fructooligosaccharides), GOS (galactooligosaccharides), and resistant starch—which support different beneficial bacterial populations. This diversity promotes a more robust, resilient gut microbiome.
- CFU count (Colony Forming Units): This indicates the number of live bacteria in each dose. Clinical trials for metabolic health and weight management typically use 10-20 billion CFU daily, though some studies show benefits at lower doses for certain strains [5]. Higher isn't automatically better; the optimal amount depends on the specific strains and your individual needs. Avoid products with vague descriptions like "probiotic blend" without specific CFU counts per strain.
- Viability and stability: Ensure the product maintains potency through its expiration date. Some probiotics require refrigeration to remain viable, while others use stabilization technologies that allow room-temperature storage. Check the label for storage requirements and guaranteed potency at expiration rather than at manufacture.
- Additional beneficial ingredients: Some formulations include digestive enzymes, vitamins (particularly B vitamins and vitamin D), or other compounds that may enhance the overall benefits for metabolic health and craving control.
- Your specific health goals: If managing sugar cravings represents your primary concern, prioritize products or dietary approaches featuring strains that have been specifically studied for effects on glucose metabolism, appetite control, body composition, or eating behaviors.
- Duration expectations: Probiotics begin colonizing your gut within 4-5 days, but meaningful metabolic benefits typically emerge at 8-12 weeks of consistent use [5]. Clinical trials for weight management and craving reduction consistently use 12-week interventions, suggesting this represents the minimum timeframe for assessing effectiveness.
It's always advisable to consult with a healthcare professional—such as a physician, registered dietitian, or naturopathic doctor—before starting any new supplement regimen. They can help you select a probiotic and prebiotic combination tailored to your individual needs, considering your medical history, current medications, existing health conditions, and specific health goals.
Probiotic Supplements vs. Fermented Foods: Which Approach Works Best?
Both probiotic supplements and fermented foods offer distinct advantages for improving gut health and managing sugar cravings. Understanding the benefits of each approach can help you make informed choices:
Probiotic Supplements
Advantages:
- Higher CFU concentrations: Typically provide 10-50 billion CFU per dose, matching levels used in clinical trials
- Strain-specific targeting: Allow you to select specific, well-researched strains for particular health goals (e.g., L. gasseri BNR17 for metabolic health)
- Better survival rates: Many use enteric coating or microencapsulation technologies that protect bacteria through stomach acid, ensuring more viable bacteria reach your intestines
- Standardized dosing: Provide consistent, measurable amounts of specific strains
- Convenience: Easy to incorporate into daily routines, especially when traveling
- Allergen-free options: Available for people with dairy sensitivities or other food allergies
Considerations:
- Cost: Typically $0.50-$2.00 per day for quality products
- Require consistent daily use for sustained benefits
- Effects diminish if supplementation stops, as most strains don't permanently colonize
Fermented Foods
Advantages:
- Greater bacterial diversity: Naturally contain 100+ different bacterial strains in foods like kefir, providing broader microbiome support than single-strain or multi-strain supplements [33]
- Additional nutrients: Deliver vitamins (especially K2 and B vitamins), minerals, beneficial enzymes, and bioactive compounds beyond just probiotics
- Natural prebiotic pairing: Often contain fiber or other compounds that feed the probiotics, creating natural synbiotic effects
- Cost-effective: Generally less expensive than high-quality supplements when incorporated as regular foods
- Sustainable: Part of traditional diets across many cultures, representing a whole-food approach
- Culinary variety: Offer diverse flavors and textures that can enhance meals
Considerations:
- Lower CFU counts per serving: Typically 1-100 million CFU per serving (though kefir can contain billions)
- Bacterial strains present may not be well-characterized or strain-specific
- Require consistent consumption and may be less convenient
- Some people dislike the taste of fermented foods
- Quality varies significantly between brands and preparation methods
Evidence-Based Recommendation
The Stanford Fermented Foods Study provides compelling guidance. Researchers assigned healthy adults to either a high-fermented-foods diet or a high-fiber diet for 10 weeks. The fermented foods group showed increased gut microbiome diversity, decreased 19 inflammatory markers (including IL-6), and improvements in immune function—all in a dose-dependent manner, meaning those who consumed the most fermented foods saw the greatest benefits [18].
Optimal strategy: Combine both approaches. Use fermented foods as your foundation for daily microbiome diversity and nutritional benefits, while adding targeted probiotic supplements when you have specific health goals like managing sugar cravings, reducing visceral fat, or supporting metabolic health. This combination provides both the broad-spectrum diversity of fermented foods and the concentrated, strain-specific effects of supplements.
The Greek Yogurt Advantage: Your Probiotic Protein Powerhouse
Greek yogurt deserves special attention as a highly accessible, nutritious source of probiotics that can be incorporated into daily eating patterns. When selecting Greek yogurt for probiotic benefits, look for these key features:
- "Live and Active Cultures" seal: This National Yogurt Association seal guarantees the product contains at least 100 million CFU per gram at the time of manufacture. This translates to billions of beneficial bacteria in a typical 6-ounce serving.
- Specific strain information: Some brands now list the specific Lactobacillus and Bifidobacterium strains used. Lactobacillus gasseri BNR17, which has been specifically studied for reducing visceral fat accumulation and supporting metabolic health, is found in certain Greek yogurt products [19].
- Minimal processing: Avoid products labeled "Greek-style" or "Greek yogurt product," which may be regular yogurt thickened with starches or thickeners rather than traditionally strained. These often lack the protein content and may have fewer live cultures.
- Avoid heat-treated yogurt: If the label says "heat-treated after culturing," the beneficial bacteria have been killed. This is sometimes done to extend shelf life but eliminates probiotic benefits.
- Plain varieties: Flavored Greek yogurts often contain substantial added sugars (10-20 grams per serving), which can feed harmful bacteria and counteract your craving-control goals. Choose plain Greek yogurt and add your own fresh fruit, a small drizzle of honey, or cinnamon for flavor.
- Protein content: Greek yogurt provides approximately 15-20 grams of protein per 6-ounce serving, which enhances satiety and helps stabilize blood sugar—both factors that reduce sugar cravings throughout the day.
Create synbiotic combinations: Maximize benefits by pairing Greek yogurt with prebiotic foods. Try these combinations:
- Greek yogurt + mixed berries + ground flaxseed (provides pectin, resistant starch, and additional fiber)
- Greek yogurt + banana + chopped walnuts (provides resistant starch, omega-3s, and polyphenols)
- Greek yogurt + chia seeds + cinnamon (provides soluble fiber and blood sugar-stabilizing cinnamon)
A daily serving of high-quality Greek yogurt can provide meaningful probiotic support while contributing to your protein intake and offering a satisfying, versatile food that helps reduce cravings for less nutritious snacks.
Building Your Fermented Foods Foundation: A Practical Implementation Plan
Incorporating fermented foods into your diet represents one of the most effective, evidence-based strategies for supporting gut health and managing sugar cravings. Based on the Stanford fermented foods study [18], here's a progressive implementation plan:
Week 1-2: Foundation Phase
Goal: Introduce one fermented food daily
Start with the most palatable option for you:
- Greek yogurt with live cultures: 6 ounces daily with breakfast or as a snack. Choose plain varieties and add fresh fruit for natural sweetness.
- Kefir: 4-8 ounces daily. Kefir contains 30-60 different bacterial strains and can be consumed plain, blended into smoothies, or used as a base for overnight oats.
Why this works: Starting gradually allows your gut bacteria and digestive system to adapt, minimizing potential gas or bloating that can occur when dramatically increasing fermented food intake.
Week 3-4: Expansion Phase
Goal: Add a second fermented food variety
Introduce:
- Kombucha: 4-8 ounces with lunch or as an afternoon beverage. Choose varieties with less than 5 grams of sugar per serving to avoid counterproductive sugar intake.
- Sauerkraut or kimchi: 2-4 tablespoons daily with meals. Start with smaller amounts as these can be quite potent.
Tip: Don't heat fermented vegetables, as high temperatures kill beneficial bacteria. Add them to meals after cooking or enjoy them cold.
Week 5-6: Diversification Phase
Goal: Rotate through various fermented foods
Add variety with:
- Fermented pickles: Look for refrigerated varieties made with salt brine rather than vinegar, as these contain live cultures. Vinegar-pickled products don't provide probiotic benefits.
- Miso: Add 1-2 tablespoons to broths, dressings, or sauces. Again, add after cooking to preserve live cultures.
- Tempeh: 3-4 ounces as a protein source 2-3 times weekly. Tempeh is fermented soybeans and provides both probiotics and complete protein.
Week 7-8 and Beyond: Optimization Phase
Goal: Achieve 2-3 servings of fermented foods daily
Establish sustainable habits:
- Morning: Greek yogurt or kefir with prebiotic-rich additions (berries, banana, flaxseed)
- Lunch or dinner: Sauerkraut, kimchi, or fermented pickles as a side
- Throughout the day: Kombucha or additional fermented vegetables as desired
Target: Aim for 2-3 servings daily for optimal benefit, as the Stanford study showed dose-dependent improvements in gut microbiome diversity and inflammatory marker reduction.
Critical Success Factors
- Consistency matters: Daily consumption provides the most significant benefits, as most probiotic bacteria don't permanently colonize your gut and require regular intake.
- Variety amplifies benefits: Different fermented foods contain different bacterial strains, so rotating through diverse options creates a more robust, diverse microbiome.
- Pair with prebiotics: Always combine fermented foods with prebiotic fibers from vegetables, fruits, whole grains, and legumes to feed the beneficial bacteria you're introducing.
- Be patient: Meaningful changes in gut microbiome composition take 4-8 weeks. Metabolic benefits like reduced cravings typically emerge at 8-12 weeks with consistent intake.
- Quality matters: Choose refrigerated, unpasteurized fermented foods when possible. Shelf-stable versions are often heat-treated, which kills beneficial bacteria.
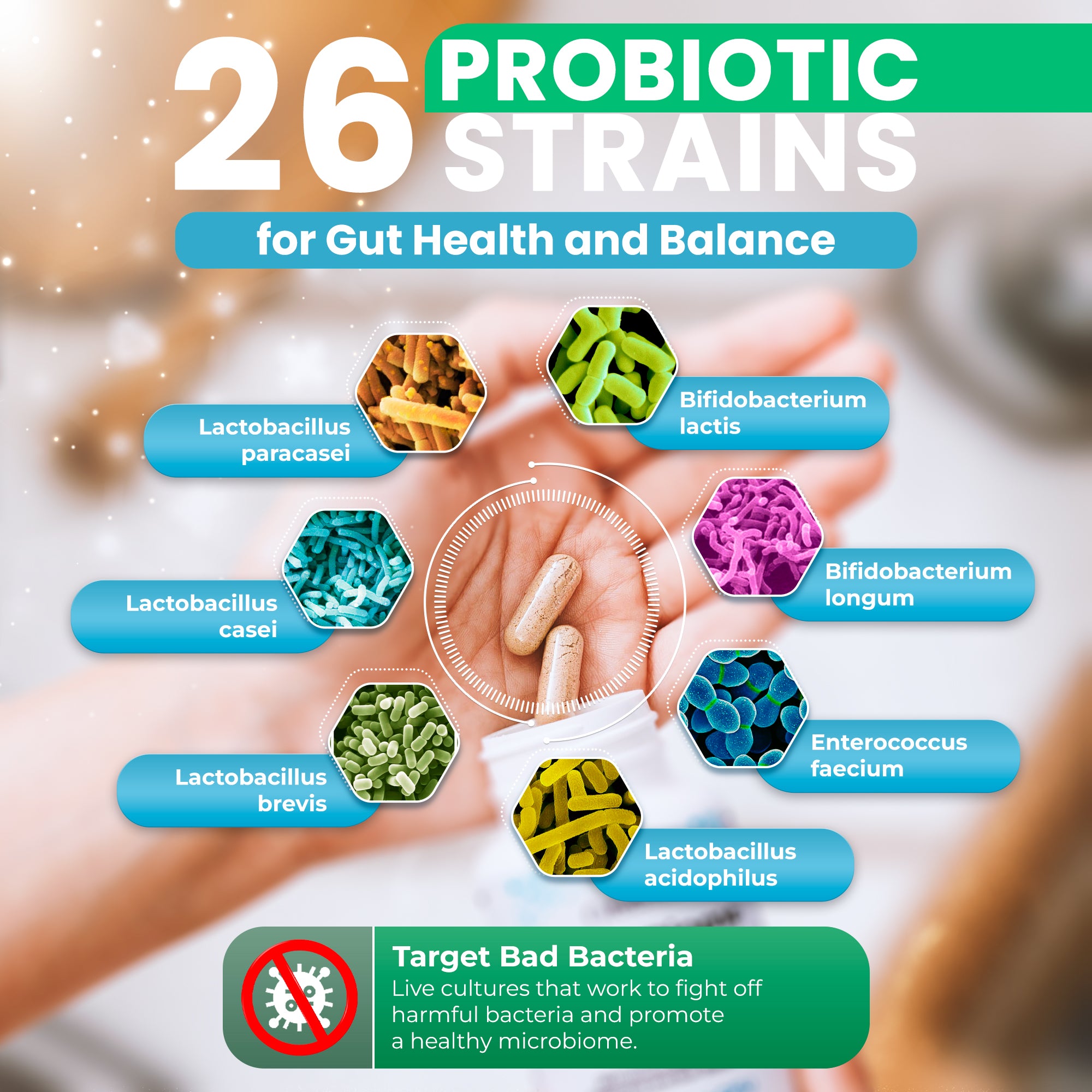
Introducing MicroBiome Restore™
Having explored how probiotics and prebiotics can help manage sugar cravings through multiple scientific pathways, let's examine a comprehensive supplement designed to support these mechanisms: MicroBiome Restore™. This gut health supplement is formulated to promote overall digestive wellness and may help manage sugar cravings by fostering a balanced and diverse gut microbiome.
MicroBiome Restore™ offers:
- 26 different probiotic strains: This diverse array of beneficial bacteria is designed to support multiple aspects of gut health, potentially influencing everything from digestion to mood regulation and craving control. The formula includes strains from the Lactobacillus, Bifidobacterium, and other genera known to support metabolic health.
- 9 organic prebiotics, including Jerusalem artichoke inulin: These carefully selected prebiotic fibers serve as nourishment for the probiotic strains, helping them survive, colonize, and thrive in your gut environment. The inclusion of Jerusalem artichoke inulin is particularly relevant, as this compound has been shown to promote beneficial bacteria growth and may help stabilize blood sugar levels.
- No fillers or artificial additives: The product is formulated with purity and potency in mind, avoiding unnecessary ingredients that could interfere with probiotic viability or trigger sensitivities.
This comprehensive combination is designed to support overall gut health and microbial diversity, which may help manage sugar cravings through several evidence-based pathways:
- Improved glucose metabolism: The formula includes probiotic strains associated with better insulin sensitivity and blood sugar regulation, potentially reducing the sudden glucose drops that trigger intense cravings for sweets.
- Enhanced intestinal barrier function: By supporting a stronger gut lining, the supplement may help reduce inflammatory signaling that amplifies cravings and disrupts normal appetite regulation.
- Increased production of beneficial compounds: The fermentation of prebiotics by probiotics produces short-chain fatty acids, which have been linked to improved metabolic health, increased satiety hormone production, and potentially reduced sugar cravings.
- Optimized gut-brain axis communication: By promoting a healthier gut environment with greater bacterial diversity, MicroBiome Restore™ may help optimize the bidirectional communication between gut and brain that influences appetite regulation, reward processing, and food preferences.
While individual results will vary based on factors like baseline gut health, diet quality, stress levels, and genetic factors, incorporating a comprehensive synbiotic supplement like MicroBiome Restore™ into a balanced diet and healthy lifestyle could provide meaningful support for gut health goals and sugar craving management.
Lifestyle Changes to Support Gut Health and Amplify Probiotic Benefits
While probiotics and prebiotics offer powerful support for gut health and sugar craving management, they work most effectively as components of a comprehensive healthy lifestyle. Making strategic changes in your daily habits can dramatically enhance the effectiveness of probiotics and prebiotics, creating an environment where beneficial gut bacteria thrive. Here are evidence-based lifestyle strategies:
- Eat a colorful variety of fruits and vegetables: Aim to include many different colors in your diet to obtain a wide spectrum of nutrients, fibers, and polyphenols that support diverse beneficial bacteria. Each color family provides different prebiotic fibers and plant compounds that feed specific bacterial populations. Target 8-10 servings daily, with emphasis on variety over volume.
- Stay well-hydrated: Adequate water intake is essential for maintaining the mucus lining of your intestines, which provides habitat and nourishment for beneficial bacteria. The mucus layer also serves as a protective barrier between your gut contents and intestinal cells. Aim for approximately half your body weight in ounces daily (e.g., 75 ounces for a 150-pound person), adjusting for activity level and climate.
- Exercise regularly: Physical activity has been shown to increase the diversity of gut bacteria and promote the growth of beneficial species, particularly those that produce butyrate and other beneficial SCFAs [34]. Research shows that regular exercise (at least 150 minutes of moderate activity weekly) positively influences gut microbiota composition independent of diet. The benefits appear within 6 weeks of starting a consistent exercise program.
- Manage stress effectively: Chronic stress is one of the most powerful disruptors of gut microbiome health. Incorporate stress-reduction practices like yoga, meditation, deep breathing exercises, progressive muscle relaxation, or mindfulness training. Even 10-15 minutes daily of these practices can help reduce stress-induced disruptions to your gut microbiota and decrease cortisol-driven sugar cravings [30].
- Prioritize quality sleep: Aim for 7-9 hours of sleep nightly to support the natural circadian rhythms of your gut bacteria. Irregular sleep schedules and chronic sleep deprivation rapidly alter gut microbiota composition, reduce beneficial bacteria populations, and intensify sugar cravings [31]. Establish consistent bed and wake times, even on weekends, to maintain stable bacterial rhythms.
- Limit processed foods and artificial sweeteners: Ultra-processed foods and artificial sweeteners (particularly saccharin, sucralose, and aspartame) can negatively impact gut bacterial diversity and potentially increase sugar cravings by altering taste preferences and metabolic signaling [35]. Focus on whole, minimally processed foods as much as practically possible.
- Include fermented foods beyond supplements: As discussed earlier, foods like kimchi, sauerkraut, kefir, miso, and tempeh provide natural probiotics with beneficial diversity to complement your supplement regimen. They also contribute additional nutrients and bioactive compounds that supplements alone cannot provide.
- Practice mindful eating: Pay attention to physical hunger and fullness cues, eat slowly without distractions, and savor your food. Mindful eating practices have been shown to reduce binge eating, improve digestion (by optimizing the cephalic phase of digestion), and potentially reduce cravings by increasing awareness of emotional versus physical hunger [36].
- Moderate alcohol consumption: Excessive alcohol intake can disrupt the balance of gut bacteria, damage the intestinal barrier, promote inflammation, and potentially increase sugar cravings through multiple mechanisms. If you drink alcohol, limit intake to moderate levels (up to 1 drink daily for women, 2 for men) and include alcohol-free days throughout the week.
- Consider time-restricted eating: Some research suggests that confining your eating to a consistent 8-12 hour window each day may help optimize circadian rhythms of your gut bacteria, improve metabolic health, and potentially reduce cravings [37]. This doesn't necessarily mean eating less food—just consuming it within a shorter daily timeframe.
- Avoid unnecessary antibiotics: While antibiotics are essential for treating bacterial infections, they also kill beneficial gut bacteria indiscriminately. Only use antibiotics when truly medically necessary, complete the full course as prescribed, and consider probiotic supplementation during and after antibiotic treatment (separated by at least 2 hours from antibiotic doses).
- Spend time in nature: Exposure to diverse natural environments may increase the diversity of your gut microbiome by exposing you to a wider variety of environmental bacteria and reducing stress. Regular time outdoors, gardening, or interacting with pets can contribute to microbiome health.
Learn more about enhancing probiotic effectiveness through lifestyle changes and additional nutritional support. Remember that consistency and patience are key when it comes to gut health. Small, sustainable changes implemented over time often lead to more significant, lasting improvements than dramatic overhauls that prove difficult to maintain. Even incremental progress—like adding one fermented food daily or taking a 15-minute walk after meals—can meaningfully benefit your gut microbiome and overall wellbeing.
Conclusion: A Holistic Approach to Managing Sugar Cravings
Probiotics and prebiotics offer a scientifically-validated approach to managing sugar cravings by supporting and optimizing your gut microbiome health. By fostering a diverse and balanced community of beneficial bacteria, you may find it substantially easier to resist sugary treats and make healthier food choices overall. The research is compelling: specific probiotic strains can reduce sugar consumption by 19%, with 91% of users reporting fewer food cravings [1] [12] [15].
However, it's essential to recognize that everyone's gut microbiome is unique—influenced by genetics, early life experiences, diet history, medications, stress levels, and numerous other factors. What works exceptionally well for one person may produce different results for another, though the fundamental principles of gut health apply universally.
The journey to better gut health and reduced sugar cravings extends beyond simply taking probiotics and prebiotics. It encompasses mindful eating habits, stress management techniques, prioritizing quality sleep, engaging in regular physical activity, and choosing whole foods over ultra-processed options. Supplements like MicroBiome Restore™ can serve as valuable tools in this comprehensive approach, providing a well-formulated combination of probiotics and prebiotics specifically designed to support overall gut health and metabolic function.
If you're struggling with persistent sugar cravings despite dietary and lifestyle efforts, consider consulting a healthcare professional about incorporating probiotics and prebiotics into your wellness strategy. They can provide personalized recommendations based on your individual health status, medical history, and specific goals, helping you develop a comprehensive plan for managing cravings and optimizing gut health.
By taking a holistic, whole-body approach to gut health, you're addressing far more than sugar cravings—you're supporting your overall health and wellbeing. The gut microbiome plays crucial roles in immune function, mental health, metabolic regulation, inflammation control, and countless other aspects of human health, making it a foundational focus for total wellness.
Remember that meaningful, sustainable changes in gut health and craving patterns take time. Most clinical trials show significant benefits emerging at 8-12 weeks of consistent intervention. Be patient with the process, stay consistent with your chosen strategies, and pay attention to how your body responds. Small, incremental improvements compound over time into substantial transformations in your relationship with food, your cravings, and your overall health.
Start improving your gut health today by incorporating fermented foods, prebiotic-rich vegetables, and targeted probiotic supplements if appropriate. You might find those intense sugar cravings becoming progressively easier to manage, replaced by genuine satisfaction from nourishing whole foods that support your health goals. The potential benefits to your overall health, energy levels, mood, and wellbeing make this journey well worth the sustained effort.
Gut Health and Sugar Cravings Improvement Timeline
Start improving your gut health today, and you might find those sugar cravings becoming easier to handle over time. Remember, being consistent and patient is important – big changes in gut health and cravings can take time, but the potential benefits to your overall health and well-being are worth the effort.
References
- Zhang T, Wang W, Li J, et al. Free fatty acid receptor 4 modulates dietary sugar preference via the gut microbiota. Nature Microbiology. 2025;10:348-361. DOI: 10.1038/s41564-024-01902-8
- Duan H, Pan J, Guo M, et al. The Mechanism of the Gut-Brain Axis in Regulating Food Intake. Nutrients. 2023;15(17):3728. DOI: 10.3390/nu15173728
- Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front Endocrinol (Lausanne). 2020;11:25. DOI: 10.3389/fendo.2020.00025
- Claus SP, Guillou H, Ellero-Simatos S. The gut microbiota: a major player in the toxicity of environmental pollutants? NPJ Biofilms Microbiomes. 2016;2:16003. DOI: 10.1038/npjbiofilms.2016.3
- Bahari H, Akhgarjand C, Mirmohammadali SN, et al. Probiotics and eating disorders: a systematic review of humans and animal model studies. J Eat Disord. 2024;12:193. DOI: 10.1186/s40337-024-01143-4
- Volkow ND, Wang GJ, Baler RD. Reward, dopamine and the control of food intake: implications for obesity. Trends Cogn Sci. 2011;15(1):37-46. DOI: 10.1016/j.tics.2010.11.001
- McDougle M, de Araujo A, Singh A, et al. Separate gut-brain circuits for fat and sugar reinforcement combine to promote overeating. Cell Metab. 2024;36(2):393-407.e7. DOI: 10.1016/j.cmet.2023.12.014
- Dicks LMT, Hurn D, Hermanus D. Gut Bacteria and Neurotransmitters. Microorganisms. 2022;10(9):1838. DOI: 10.3390/microorganisms10091838
- Ivezaj V, Grilo CM. The complexity of body image following bariatric surgery: a systematic review of the literature. Obes Rev. 2018;19(8):1116-1140. DOI: 10.1111/obr.12685
- Aguirre M, Bussolo de Souza C, Venema K. The Gut Microbiota from Lean and Obese Subjects Contribute Differently to the Fermentation of Arabinogalactan and Inulin. PLoS One. 2016;11(7):e0159236. DOI: 10.1371/journal.pone.0159236
- Carlos LO, Ramos MRZ, Wagner NRF, et al. Probiotic supplementation attenuates binge eating and food addiction 1 year after Roux-en-Y gastric bypass: a randomized, double-blind, placebo-controlled trial. Arq Bras Cir Dig. 2022;35:e1659. DOI: 10.1590/0102-672020210002e1659
- Liu E, Ji X, Zhou K. Akkermansia muciniphila for the Prevention of Type 2 Diabetes and Obesity: A Meta-Analysis of Animal Studies. Nutrients. 2024;16(20):3440. DOI: 10.3390/nu16203440
- Canfora EE, Jocken JW, Blaak EE. Short-chain fatty acids in control of body weight and insulin sensitivity. Nat Rev Endocrinol. 2015;11(10):577-591. DOI: 10.1038/nrendo.2015.128
- Parnell JA, Reimer RA. Prebiotic fibres dose-dependently increase satiety hormones and alter bacteroidetes and firmicutes in lean and obese JCR:LA-cp rats. Br J Nutr. 2012;107(4):601-613. DOI: 10.1017/S0007114511003163
- Fetissov SO, Legrand R, Lucas N. Lactobacillus salivarius and Lactobacillus gasseri supplementation reduces stress-induced sugar craving in mice. Eur Eat Disord Rev. 2023;31(4):745-758. DOI: 10.1002/erv.3004
- Zhang W, Jiao L, Liu R, et al. From gut microbiota to host appetite: gut microbiota-derived metabolites as key regulators. Microbiome. 2021;9:162. DOI: 10.1186/s40168-021-01093-y
- Furman D, Campisi J, Verdin E, et al. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019;25(12):1822-1832. DOI: 10.1038/s41591-019-0675-0
- Wastyk HC, Fragiadakis GK, Perelman D, et al. Gut-microbiota-targeted diets modulate human immune status. Cell. 2021;184(16):4137-4153.e14. DOI: 10.1016/j.cell.2021.06.019
- Kim J, Yun JM, Kim MK, et al. Lactobacillus gasseri BNR17 Supplementation Reduces the Visceral Fat Accumulation and Waist Circumference in Obese Adults: A Randomized, Double-Blind, Placebo-Controlled Trial. J Med Food. 2018;21(5):454-461. DOI: 10.1089/jmf.2017.3937
- Park DY, Ahn YT, Park SH, et al. Anti-Obesity Effect of Lactobacillus gasseri BNR17 in High-Sucrose Diet-Induced Obese Mice. PLoS One. 2013;8(1):e54617. DOI: 10.1371/journal.pone.0054617
- Plovier H, Everard A, Druart C, et al. A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Nat Med. 2017;23(1):107-113. DOI: 10.1038/nm.4236
- Depommier C, Everard A, Druart C, et al. Supplementation with Akkermansia muciniphila in overweight and obese human volunteers: a proof-of-concept exploratory study. Nat Med. 2019;25(7):1096-1103. DOI: 10.1038/s41591-019-0495-2
- Minami J, Kondo S, Yanagisawa N, et al. Effects of Bifidobacterium breve B-3 on body fat reductions in pre-obese adults: a randomized, double-blind, placebo-controlled trial. Biosci Microbiota Food Health. 2018;37(3):67-75. DOI: 10.12938/bmfh.18-001
- Guess ND, Dornhorst A, Oliver N, et al. A Randomized Controlled Trial: The Effect of Inulin on Weight Management and Ectopic Fat in Subjects with Prediabetes. Nutr Metab (Lond). 2015;12:36. DOI: 10.1186/s12986-015-0033-2
- Canfora EE, van der Beek CM, Jocken JWE, et al. Colonic infusions of short-chain fatty acid mixtures promote energy metabolism in overweight/obese men: a randomized crossover trial. Sci Rep. 2017;7(1):2360. DOI: 10.1038/s41598-017-02546-x
- Bischoff SC, Barbara G, Buurman W, et al. Intestinal permeability--a new target for disease prevention and therapy. BMC Gastroenterol. 2014;14:189. DOI: 10.1186/s12876-014-0189-7
- Zeng F, He L, Wang K, et al. Crosstalk between glucagon-like peptide 1 and gut microbiota in metabolic diseases. mBio. 2024;15(1):e02032-23. DOI: 10.1128/mbio.02032-23
- Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91(4):449-458. DOI: 10.1016/j.physbeh.2007.04.011
- Bharwani A, Mian MF, Foster JA, et al. Structural & functional consequences of chronic psychosocial stress on the microbiome & host. Psychoneuroendocrinology. 2016;63:217-227. DOI: 10.1016/j.psyneuen.2015.10.001
- Berding K, Bastiaanssen TFS, Moloney GM, et al. Feed your microbes to deal with stress: a psychobiotic diet impacts microbial stability and perceived stress in a healthy adult population. Mol Psychiatry. 2023;28:601-610. DOI: 10.1038/s41380-022-01817-y
- Smith RP, Easson C, Lyle SM, et al. Gut microbiome diversity is associated with sleep physiology in humans. PLoS One. 2019;14(10):e0222394. DOI: 10.1371/journal.pone.0222394
- Spiegel K, Tasali E, Penev P, et al. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846-850. DOI: 10.7326/0003-4819-141-11-200412070-00008
- Bourrie BCT, Willing BP, Cotter PD. The Microbiota and Health Promoting Characteristics of the Fermented Beverage Kefir. Front Microbiol. 2016;7:647. DOI: 10.3389/fmicb.2016.00647
- Monda V, Villano I, Messina A, et al. Exercise Modifies the Gut Microbiota with Positive Health Effects. Oxid Med Cell Longev. 2017;2017:3831972. DOI: 10.1155/2017/3831972
- Suez J, Korem T, Zeevi D, et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature. 2014;514(7521):181-186. DOI: 10.1038/nature13793
- Warren JM, Smith N, Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: effectiveness and associated potential mechanisms. Nutr Res Rev. 2017;30(2):272-283. DOI: 10.1017/S0954422417000154
- Chaix A, Manoogian ENC, Melkani GC, et al. Time-Restricted Eating to Prevent and Manage Chronic Metabolic Diseases. Annu Rev Nutr. 2019;39:291-315. DOI: 10.1146/annurev-nutr-082018-124320










Share and get 15% off!
Simply share this product on one of the following social networks and you will unlock 15% off!