Bifidobacterium Deficiency: Understanding the Missing Microbes Affecting Modern Gut Health
In the first few months of life, a healthy infant's gut should be dominated by Bifidobacterium—beneficial bacteria that colonize the intestines, train the developing immune system, and lay the foundation for lifelong health. Yet groundbreaking research from 2025 reveals a troubling reality: approximately 25% of infants in the United States lack detectable Bifidobacterium in their gut microbiome.[1] This widespread deficiency doesn't disappear with age—it persists through childhood, adulthood, and into our later years, contributing to rising rates of allergies, autoimmune conditions, inflammatory disorders, and metabolic dysfunction. Understanding Bifidobacterium deficiency, its causes, and evidence-based restoration strategies has never been more critical for supporting optimal gut health across the human lifespan.
Key Takeaways
- Approximately 25% of U.S. infants lack detectable Bifidobacterium, with deficiency rates reaching 35% among cesarean-section births compared to 19% in vaginal births[1]
- Infants deficient in Bifidobacterium face a three-fold increased risk of developing allergies, asthma, or eczema by age two[2]
- Bifidobacterium populations decline naturally with age, from 90% of infant gut microbiota to 5-10% in elderly adults, making restoration important across the lifespan[3]—our guide to probiotics for men over 40 covers how to address this with clinically studied strains
- Depletion or absence of Bifidobacterium is associated with autoimmune responses, impaired immune homeostasis, inflammatory conditions, and metabolic disorders[4]
- Multi-strain probiotic supplementation featuring diverse Bifidobacterium species (B. longum, B. lactis, B. breve, B. infantis, B. bifidum) alongside organic prebiotics offers a comprehensive approach to microbiome restoration
Understanding Bifidobacterium: The Foundation of Gut Health
Bifidobacterium is a genus of beneficial bacteria belonging to the Actinobacteria phylum, first identified over a century ago by French pediatrician Henry Tissier who observed their abundance in the feces of healthy breastfed infants.[5] These gram-positive, anaerobic bacteria have evolved alongside humans for millennia, establishing themselves as among the earliest and most important colonizers of the human gut immediately following birth.
What makes Bifidobacterium so crucial to human health extends far beyond simple colonization. These bacteria perform multiple essential functions: they ferment dietary fibers and human milk oligosaccharides (HMOs) that our own digestive enzymes cannot break down, producing beneficial short-chain fatty acids like acetate and lactate that nourish intestinal cells and modulate immune function.[6] They synthesize certain B vitamins essential for cellular metabolism. They compete with pathogenic bacteria for colonization sites and nutrients, creating what scientists call "colonization resistance" that protects against harmful microbes.[7] Perhaps most importantly, Bifidobacterium species interact directly with our immune cells—training regulatory T cells, maintaining intestinal barrier integrity, and dampening excessive inflammatory responses that can lead to chronic disease.
The genus Bifidobacterium contains more than 50 identified species, but only about a dozen regularly inhabit the human gut. These species show remarkable age-specificity: B. breve, B. longum subsp. infantis, and B. bifidum predominate in healthy infants, while B. longum subsp. longum, B. adolescentis, and B. catenulatum become more prevalent during adulthood.[8] This age-related species shift reflects metabolic adaptation to changing dietary patterns, with infant-associated species specialized for processing milk components and adult-associated species better equipped to ferment complex plant fibers.
The Lifecycle of Bifidobacterium Populations
In healthy development, Bifidobacterium follows a predictable population trajectory. During the first days following birth—particularly after vaginal delivery—pioneer species like B. breve and B. longum subsp. infantis rapidly colonize the infant gut, aided by exposure to maternal vaginal and fecal microbiota.[9] By one to three months of age, Bifidobacterium can constitute up to 90% of total gut bacteria in exclusively breastfed infants, creating what researchers call a "Bifidobacterium-dominant microbiome."

This early dominance serves critical developmental purposes. Research demonstrates that Bifidobacterium colonization during infancy is associated with proper immune system maturation, reduced risk of atopic diseases, improved vaccine responses, and healthy metabolic programming.[10] The bacteria essentially "educate" the developing immune system, teaching it to distinguish between harmful threats and benign antigens—a process that when disrupted can predispose individuals to allergic and autoimmune conditions later in life.
As weaning progresses and solid foods are introduced, Bifidobacterium populations naturally decrease as gut microbial diversity increases. By adulthood, Bifidobacterium typically comprises 10-40% of the gut microbiota in healthy individuals—still substantial but no longer dominant.[3] The species composition also shifts, with adult-type Bifidobacterium (particularly B. longum and B. adolescentis) replacing infant-type species as dietary carbohydrates change from milk-based to plant-based sources.
In elderly populations, Bifidobacterium abundance declines further to approximately 5% of gut microbiota, coinciding with age-related changes in immune function, increased inflammatory markers, and higher susceptibility to infections.[11] This age-related decline, termed "inflammaging," may be partially driven by or exacerbated by Bifidobacterium depletion, creating a vicious cycle of microbial dysbiosis and chronic low-grade inflammation.
The Widespread Deficiency: Causes and Populations at Risk
The alarming finding that one in four U.S. infants lacks detectable Bifidobacterium represents a dramatic departure from historical norms and raises urgent questions about what's driving this widespread deficiency. The My Baby Biome study—the largest cross-sectional analysis of the U.S. infant gut microbiome to date—examined stool samples from 412 demographically representative infants aged one to three months using advanced metagenomic and metabolomic profiling.[1] The results paint a concerning picture of microbial disruption affecting infants regardless of feeding method, geographic location, or socioeconomic status.
Birth Mode as a Critical Factor
Among the study's most significant findings: cesarean section delivery substantially increases Bifidobacterium deficiency risk. While 19% of vaginally delivered infants showed Bifidobacterium deficit, this rate jumped to 35% among C-section infants—nearly double the risk.[1] This disparity reflects the importance of vaginal birth's microbial transfer, where infants are inoculated with maternal vaginal and intestinal bacteria as they pass through the birth canal.
C-section infants, bypassing this natural microbial seeding, often show delayed and reduced Bifidobacterium colonization. In many cases, potentially pathogenic bacteria occupy the ecological niche that Bifidobacterium would normally fill, particularly bacteria capable of metabolizing human milk oligosaccharides—complex sugars in breast milk specifically designed by evolution to feed beneficial bacteria like Bifidobacterium.[12] When opportunistic bacteria consume these specialized sugars instead of Bifidobacterium, infants lose both the protective benefits of beneficial bacteria and the immune-training functions that Bifidobacterium provides.
Antibiotic Exposure and Microbiome Disruption
Antibiotic administration—whether to mothers during pregnancy and delivery or to infants during early life—represents another major driver of Bifidobacterium deficiency. While antibiotics save lives by eliminating dangerous pathogens, they simultaneously decimate beneficial bacteria including Bifidobacterium species that are particularly susceptible to many common antibiotics.[13] Studies show that even single courses of antibiotics during infancy can reduce Bifidobacterium populations by 90% or more, with recovery taking months or sometimes failing to occur at all.
The impact extends beyond direct bacterial killing. Antibiotic-induced dysbiosis creates ecological opportunities for antibiotic-resistant bacteria and fungi to overgrow, establishing dysbiotic patterns that can persist for years. Research from the My Baby Biome study found that microbiomes lacking Bifidobacterium showed significantly higher levels of antimicrobial resistance genes and virulence factors compared to Bifidobacterium-dominant microbiomes.[1] This suggests that Bifidobacterium depletion doesn't just create an absence of beneficial bacteria—it actively promotes the establishment of potentially harmful microbial communities.
Dietary Factors and Modern Feeding Practices
While the My Baby Biome study found Bifidobacterium deficiency regardless of feeding method, formula feeding has historically been associated with reduced Bifidobacterium abundance compared to exclusive breastfeeding.[14] Breast milk contains not only live Bifidobacterium that transfer from mother to infant, but also human milk oligosaccharides (HMOs)—complex sugars that humans cannot digest but that specifically feed infant Bifidobacterium species, particularly B. longum subsp. infantis.

Modern infant formulas have improved dramatically, with many now incorporating prebiotics designed to mimic HMOs. However, these synthetic prebiotics don't perfectly replicate the structural diversity of natural HMOs, potentially explaining why formula-fed infants still show somewhat different Bifidobacterium profiles compared to breastfed infants. The good news from recent research is that with high-quality formulas and appropriate probiotic supplementation, formula-fed infants can achieve Bifidobacterium levels approaching those of breastfed babies.[15]
Beyond infancy, modern Western dietary patterns—characterized by low fiber intake, high processed food consumption, and limited fermented food consumption—fail to provide the prebiotic substrates that adult Bifidobacterium species need to thrive. The typical American consumes only 10-15 grams of fiber daily, far below the recommended 25-35 grams.[16] This chronic fiber deficit starves beneficial bacteria including Bifidobacterium, contributing to the progressive microbial depletion observed in industrialized populations.
Environmental and Lifestyle Factors
The "hygiene hypothesis" proposes that reduced microbial exposure in modern sanitized environments contributes to immune dysfunction and allergic disease. While proper hygiene prevents dangerous infections, excessive sterilization of living environments may limit beneficial microbial transfer that historically helped establish robust gut microbiomes.[17] Studies of Old Order Mennonite communities with traditional farming lifestyles show dramatically higher infant Bifidobacterium abundance compared to industrialized populations, suggesting that environmental microbial exposure plays important roles in early-life colonization.[18]
Chronic stress and circadian rhythm disruption also impact Bifidobacterium populations through the gut-brain axis. Research demonstrates that stress hormones can alter gut microbial composition, with Bifidobacterium populations showing particular vulnerability to chronic psychological stress.[19] The mechanisms involve stress-induced changes in intestinal motility, mucus production, and immune function that collectively create less favorable environments for beneficial bacteria.
Health Consequences of Bifidobacterium Deficiency Across the Lifespan
The absence or depletion of Bifidobacterium doesn't simply represent missing bacteria—it creates cascading consequences for immune function, metabolic health, barrier integrity, and disease risk. The My Baby Biome study's longitudinal health tracking revealed that by age two, infants lacking adequate Bifidobacterium during the first months of life faced substantially elevated risks of developing atopic conditions.[2] Approximately 30% of study participants showed signs of allergies, asthma, or eczema by their second birthday, with the two microbial community clusters showing the lowest Bifidobacterium abundance accounting for 76% of these adverse outcomes.
Immune Development and Allergic Disease
Bifidobacterium species play essential roles in training the developing immune system during the critical window of early life. At the cellular level, these bacteria upregulate suppressive regulatory T cells (Tregs)—specialized immune cells that prevent excessive inflammatory responses and maintain tolerance to harmless antigens.[4] When Bifidobacterium colonization is insufficient or absent during infancy, Treg development may be impaired, predisposing individuals to allergic sensitization and autoimmune conditions.
The mechanism involves complex interactions between bacterial metabolites and host immune cells. Bifidobacterium fermentation of dietary fibers produces short-chain fatty acids (SCFAs), particularly acetate, that signal to intestinal epithelial cells and immune cells to maintain anti-inflammatory states.[20] These SCFAs strengthen intestinal barrier function by enhancing tight junction protein expression, reducing the "leaky gut" phenomenon that allows food antigens and bacterial components to inappropriately cross into systemic circulation where they can trigger allergic or inflammatory responses.
Population studies consistently show inverse relationships between early Bifidobacterium abundance and later allergic disease development. A comprehensive analysis found that children who developed wheezing disorders showed significantly lower Bifidobacterium levels compared to healthy children, with this difference detectable even before symptoms appeared.[21] The protective effect appears dose-dependent: higher Bifidobacterium abundance correlates with progressively lower allergy risk.
Autoimmune and Inflammatory Conditions
Beyond allergic disease, Bifidobacterium deficiency has been implicated in autoimmune conditions including inflammatory bowel disease (IBD), multiple sclerosis, type 1 diabetes, and rheumatoid arthritis. Research examining Bifidobacterium's role in immune modulation demonstrates that depletion or absence of these bacteria is associated with autoimmune responses and impaired immune homeostasis.[4]
In inflammatory bowel disease, patients with Crohn's disease and ulcerative colitis consistently show reduced Bifidobacterium abundance compared to healthy controls.[22] Animal studies demonstrate that Bifidobacterium supplementation can ameliorate experimental colitis by modulating dendritic cell and macrophage activity, reducing intestinal inflammation, and promoting mucosal healing. The bacteria produce specific proteins and metabolites that interact with pattern recognition receptors on immune cells, triggering anti-inflammatory signaling cascades that dampen excessive immune activation.
Emerging research even links Bifidobacterium status to neurological autoimmune conditions. A study examining multiple sclerosis found that patients showed altered Bifidobacterium composition compared to healthy individuals, with the bacteria potentially influencing disease progression through gut-brain axis mechanisms.[23] While direct causation remains under investigation, the associations suggest that maintaining robust Bifidobacterium populations may help protect against various autoimmune pathologies.
Learn more about how the gut-brain axis impacts mental wellbeing and neurological health.
Metabolic Health and Weight Regulation
The relationship between gut microbiota and metabolic health has exploded as a research area over the past decade, with Bifidobacterium emerging as a key player in glucose metabolism, insulin sensitivity, and healthy weight maintenance. Studies show that individuals with obesity and type 2 diabetes typically have lower Bifidobacterium abundance compared to metabolically healthy individuals.[24]
The mechanisms involve multiple pathways. Bifidobacterium-produced short-chain fatty acids improve insulin sensitivity and glucose homeostasis by activating specific receptors on metabolic tissues.[25] These bacteria also reduce metabolic endotoxemia—the phenomenon where bacterial lipopolysaccharides from gram-negative bacteria leak through compromised intestinal barriers into circulation, triggering chronic low-grade inflammation that promotes insulin resistance. By maintaining barrier integrity and competing with gram-negative bacteria, Bifidobacterium helps prevent this metabolic dysfunction.
For men specifically, Bifidobacterium deficiency may have implications beyond digestive health—a 2024 study found that Bifidobacterium longum reduced prostate inflammation markers by approximately 5-fold, as detailed in our guide to probiotics for prostate support.
Bifidobacterium deficiency is particularly common in postmenopausal women, where reduced microbial diversity can worsen symptoms like mood changes, sleep disturbances, and bone loss—see our research on how probiotics support menopausal health for evidence-based solutions.
Bifidobacterium species also influence energy harvest from food, fat storage, and satiety signaling. Research demonstrates that certain Bifidobacterium strains can modulate expression of genes involved in lipid metabolism and energy expenditure, potentially explaining why individuals with robust Bifidobacterium populations tend to maintain healthier body weights even when consuming similar calories to those with depleted populations.[26]
Depleted Bifidobacterium populations — particularly B. breve and B. lactis — have been associated with increased fat accumulation in clinical research, which we cover in detail in our guide to the best probiotics for belly fat.
Cognitive Function and Mental Health
The gut-brain axis—the bidirectional communication network between the intestinal microbiome and the central nervous system—represents one of the most fascinating frontiers in microbiome research. Bifidobacterium plays important roles in this axis through multiple mechanisms: producing neuroactive metabolites including gamma-aminobutyric acid (GABA) and serotonin precursors, modulating vagus nerve signaling, reducing neuroinflammation through improved barrier function, and influencing stress hormone responses.[27]
Clinical studies show that Bifidobacterium supplementation can reduce symptoms of anxiety and depression in some individuals, improve stress resilience, and enhance cognitive performance.[28] Animal research demonstrates that mice lacking Bifidobacterium show altered stress responses, increased anxiety-like behaviors, and impaired memory formation compared to mice with healthy Bifidobacterium populations.
The age-related decline in Bifidobacterium abundance may contribute to cognitive aging and increased dementia risk in elderly populations. Observational studies have found associations between low Bifidobacterium levels and accelerated cognitive decline, though whether this relationship is causal or correlational remains under investigation.[29]
Infection Resistance and Immune Competence
Bifidobacterium's protective effects extend to resistance against acute infections. Recent research examining COVID-19 severity found that patients with severe SARS-CoV-2 infections possessed significantly lower Bifidobacterium abundance compared to individuals with mild symptoms or asymptomatic infection.[30] The study identified an inverse association between disease severity and Bifidobacterium levels, leading researchers to hypothesize that low bacterial diversity and Bifidobacterium depletion either before or after infection led to reduced immune function, allowing SARS-CoV-2 infection to become more severe.
The mechanisms involve enhanced innate immune surveillance, improved interferon responses, and maintained barrier function that reduces viral dissemination. Bifidobacterium has been shown to enhance production of antiviral cytokines while simultaneously dampening excessive inflammatory responses that can cause tissue damage during severe infections.[31]
Thyroid Function and Endocrine Health
Emerging evidence links Bifidobacterium to thyroid health through what researchers term the "gut-thyroid axis." A 2025 Mendelian randomization study found that Bifidobacterium depletion promotes goiter development through modulation of iodine metabolism.[32] The gut microbiota, particularly Bifidobacterium species, appears to regulate thyroid function through microbial metabolites—especially short-chain fatty acids—that influence expression and activity of the sodium-iodide symporter, the key transporter responsible for iodine uptake into thyroid cells.
This represents an unexpected but potentially significant consequence of Bifidobacterium deficiency, suggesting that microbiome restoration may support optimal thyroid hormone synthesis and metabolism.
Why Multi-Strain Bifidobacterium Supplementation Matters
Given the health consequences of Bifidobacterium deficiency, restoration becomes a critical therapeutic strategy. However, not all probiotic approaches offer equal benefits. The scientific literature increasingly demonstrates that multi-strain formulations providing diverse Bifidobacterium species offer advantages over single-strain products through complementary mechanisms and broader ecological support.
Species-Specific Functions and Synergies
Different Bifidobacterium species evolved to fill distinct ecological niches and perform specialized functions. Bifidobacterium longum subsp. infantis, for instance, uniquely possesses the complete genetic machinery to efficiently metabolize all types of human milk oligosaccharides—a capability that makes it the dominant species in healthy breastfed infants but that becomes less advantageous in adults consuming primarily plant-based fibers.[33]
In contrast, Bifidobacterium adolescentis and Bifidobacterium longum subsp. longum show superior ability to ferment complex plant polysaccharides including resistant starch and arabinoxylans commonly found in whole grains and vegetables—making these species particularly relevant for adult microbiome support.[34] Bifidobacterium lactis (also called B. animalis subsp. lactis) demonstrates exceptional stress tolerance and survival through gastric acid, explaining why it's the most widely used Bifidobacterium in commercial probiotics and why research on this species is particularly extensive.[35]
Bifidobacterium breve produces unique antimicrobial compounds that inhibit pathogenic bacteria while supporting intestinal barrier function, making it particularly valuable for individuals dealing with dysbiosis or chronic digestive issues.[36] Bifidobacterium bifidum, present across all life stages, shows strong adherence to intestinal mucosa and produces specific bacteriocins that create colonization resistance against harmful microbes.[37]
When multiple Bifidobacterium species are provided together, they can occupy different intestinal regions, utilize different nutrient sources, produce complementary metabolites, and collectively provide more robust ecosystem support than any single species alone. Research comparing multi-strain versus single-strain probiotics consistently demonstrates superior outcomes with diverse formulations, including better colonization, more substantial shifts in overall microbiome composition, and stronger clinical benefits.[38]
Learn more about the advantages of multi-strain probiotic formulations for comprehensive gut support.
The Prebiotic Connection: Feeding Bifidobacterium for Sustainable Colonization
Providing probiotic Bifidobacterium without adequate prebiotic substrates to feed these bacteria is like planting seeds without water—they may temporarily survive but cannot establish sustained populations. The most effective approach combines probiotics with carefully selected prebiotics in what scientists call "synbiotic" formulations.
Prebiotics are specific types of dietary fiber that resist human digestion but serve as preferred nutrition for beneficial bacteria. Different Bifidobacterium species show preferences for different prebiotic types. Inulin and fructooligosaccharides (FOS) selectively feed Bifidobacterium while being less accessible to many potentially harmful bacteria.[39] However, for individuals with sensitive digestive systems or small intestinal bacterial overgrowth (SIBO), rapidly-fermentable prebiotics like inulin can cause uncomfortable gas and bloating.
More gentle prebiotic options include partially hydrolyzed guar gum, acacia senegal gum (also called gum arabic), and certain resistant starches that ferment more slowly and in more distal regions of the colon where Bifidobacterium populations are highest.[40] Discover more about acacia senegal's unique properties for sensitive digestive systems.
Advanced formulations incorporate diverse organic prebiotic sources—jerusalem artichoke (high in inulin), fig fruit (pectin and fiber), medicinal mushrooms like maitake (beta-glucans and unique polysaccharides), and sea vegetables (alginate fibers and trace minerals).[41] This diversity ensures that multiple Bifidobacterium species receive appropriate nutrition while avoiding over-reliance on any single prebiotic that might cause digestive distress.
Read about how maitake mushroom specifically supports Bifidobacterium growth and immune function.
Delivery Systems and Bacterial Viability
Even the best probiotic strains provide no benefit if they die during manufacturing, storage, or passage through stomach acid before reaching the intestines. Bifidobacterium species are obligate anaerobes—they cannot tolerate oxygen exposure—and many strains show sensitivity to acidic conditions, making delivery technology critically important.[42]
Traditional capsule materials offer varying levels of protection. Gelatin capsules contain 13-16% moisture that can transfer to probiotic powders during storage, potentially reducing bacterial viability. Hard gelatin can also undergo cross-linking reactions from humidity or UV light that prevent proper dissolution in the digestive tract.[43] HPMC (hydroxypropyl methylcellulose) capsules provide lower moisture content but still offer limited oxygen barrier protection.
Advanced capsule technologies like pullulan—a plant-based polysaccharide produced through fermentation—provide superior oxygen barrier properties (up to 300 times better than HPMC) while offering the additional benefit of serving as a prebiotic substrate that Bifidobacterium species can ferment.[44] This dual-function approach means even the capsule material contributes to supporting beneficial bacteria rather than serving as inert packaging.
Shelf stability also depends on manufacturing conditions, packaging materials (moisture barriers, oxygen absorbers), and storage temperature. Premium formulations should remain potent at room temperature without refrigeration, making them practical for daily use and travel. When evaluating probiotics, look for products that guarantee CFU counts through expiration date rather than just at time of manufacture—this indicates the company has validated long-term stability.
For more guidance, see our comprehensive article on how to choose the best probiotic supplement for your needs.
MicroBiome Restore: A Comprehensive Approach to Bifidobacterium Restoration
At BioPhysics Essentials, we designed MicroBiome Restore specifically to address the widespread Bifidobacterium deficiency affecting modern populations. Rather than following conventional approaches that prioritize manufacturing convenience over therapeutic efficacy, we formulated every aspect of this product around a single principle: maximum support for gut microbiome restoration with zero compromises.
Five Bifidobacterium Species for Lifecycle Support
MicroBiome Restore contains five distinct Bifidobacterium species, each selected for specific functional contributions and collectively providing comprehensive support across the human lifespan:
Bifidobacterium longum subsp. longum represents the dominant Bifidobacterium species in healthy adults, showing exceptional ability to ferment complex plant polysaccharides and resistant starches common in fiber-rich diets. Research demonstrates that B. longum produces acetate and lactate that support intestinal barrier function while modulating immune responses to reduce inflammation.[45] This species also shows promising effects in the gut-brain axis, with studies indicating potential benefits for stress resilience and cognitive function. Read more about Bifidobacterium longum and its relationship with dietary sources.
Bifidobacterium lactis (B. animalis subsp. lactis) represents the most extensively researched Bifidobacterium species for probiotic applications, with hundreds of clinical studies documenting safety and efficacy. This species demonstrates exceptional survival through gastric acid and bile salts, making it particularly effective at reaching the intestines viable and ready to colonize.[46] B. lactis shows broad health benefits including immune modulation, improved intestinal transit time, reduced bloating, and enhanced barrier function. Discover the specific benefits of Bifidobacterium lactis for digestive wellness.
Bifidobacterium breve predominates in healthy breastfed infants and plays critical roles in early immune system development and allergy prevention. This species produces unique antimicrobial compounds that inhibit pathogenic bacteria while supporting intestinal epithelial integrity.[47] Research shows B. breve supplementation in preterm infants significantly reduces necrotizing enterocolitis risk and supports healthy weight gain. In adults, B. breve helps maintain the protective infant-type Bifidobacterium that declines with age, potentially offering benefits for immune function and metabolic health.
Bifidobacterium infantis (B. longum subsp. infantis) possesses specialized genetic machinery to metabolize all types of human milk oligosaccharides, making it uniquely adapted to the infant gut environment. This species has garnered significant research attention following findings that its absence in U.S. infants correlates with increased allergy and eczema risk.[1] B. infantis produces specific metabolites that train developing immune systems and establish anti-inflammatory microbial environments. Even in adults, B. infantis supplementation can provide immune-modulating benefits and compete with pathogenic bacteria for colonization sites.[48]
Bifidobacterium bifidum appears across all life stages and shows strong adherence to intestinal mucosa, where it produces bacteriocins and organic acids that create colonization resistance against harmful microbes. Research demonstrates that B. bifidum helps maintain intestinal barrier integrity, modulates immune cell function, and may provide particular benefits for individuals with irritable bowel syndrome and inflammatory conditions.[49] Learn about Bifidobacterium bifidum deficiency and its specific health implications.
Among the Bifidobacterium species most relevant to digestive health, B. infantis has particularly strong clinical evidence for IBS, with multiple randomized controlled trials demonstrating significant symptom relief.
By incorporating all five species, MicroBiome Restore addresses the diverse metabolic and functional needs of Bifidobacterium restoration—from infant-type species that may have been absent during critical developmental windows to adult-type species optimized for contemporary dietary patterns.
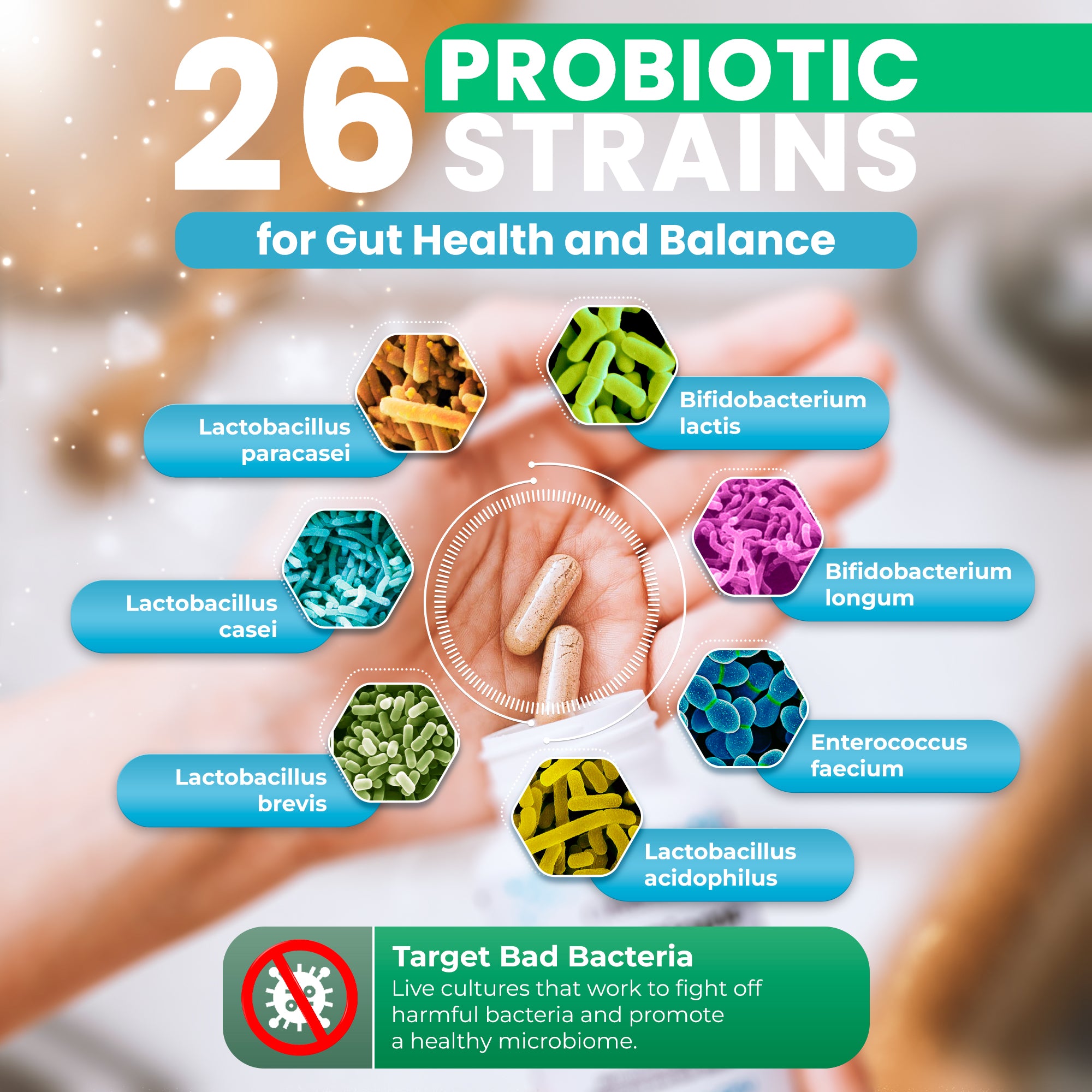
Beyond Bifidobacterium: 26 Total Strains for Comprehensive Microbiome Support
While Bifidobacterium restoration represents a primary focus, optimal gut health requires broader microbial diversity. MicroBiome Restore delivers 26 total probiotic strains including multiple Lactobacillus species (now reclassified under updated taxonomy as Lactiplantibacillus, Lacticaseibacillus, and related genera), soil-based organisms (Bacillus species), and other beneficial bacteria that work synergistically with Bifidobacterium to create a balanced, resilient microbiome.[50]
This diversity matters because different bacterial genera occupy different intestinal niches, utilize different nutrient sources, produce different metabolites, and provide complementary protective and metabolic functions. Soil-based organisms like Bacillus coagulans and Bacillus subtilis, for instance, exist in spore form that provides exceptional stability and acid resistance, allowing them to survive storage and gastric passage more readily than vegetative bacteria.[51] Learn more about soil-based organisms and their unique probiotic benefits.
The result is a formulation that doesn't just replace missing Bifidobacterium but rebuilds entire microbiome ecosystem diversity—the foundation of long-term digestive and systemic health.
Nine Organic Prebiotics: Nutrition for Sustainable Colonization
MicroBiome Restore incorporates nine certified organic prebiotic ingredients specifically selected to feed diverse Bifidobacterium species while supporting overall gut health:
Jerusalem Artichoke provides high inulin content—a fructan prebiotic that Bifidobacterium species preferentially ferment. Inulin supports increased Bifidobacterium abundance, improved calcium absorption, and enhanced production of beneficial short-chain fatty acids.[52] For more on inulin's benefits during special physiological states, read about inulin supplementation during pregnancy.
Fig Fruit offers soluble and insoluble fiber, antioxidant compounds, and natural prebiotics that support gentle digestive function while feeding beneficial bacteria. Figs provide pectin—a prebiotic fiber that ferments more slowly than inulin, reducing the bloating and gas that rapidly-fermentable prebiotics can cause in sensitive individuals.
Maitake Mushroom contains beta-glucans and unique polysaccharides that stimulate growth of both Lactobacillus and Bifidobacterium strains while encouraging short-chain fatty acid production. Maitake also provides immune-stimulating proteoglycans that enhance the immunomodulatory effects of probiotic bacteria.[53]
Acacia Senegal (gum arabic) offers highly soluble fiber that's low-FODMAP friendly and gentle on sensitive digestive systems. Acacia promotes healthy gut barrier function by encouraging short-chain fatty acid production while being well-tolerated even by individuals with IBS or SIBO who react poorly to other prebiotics.[54] See our detailed guide on acacia's unique benefits for sensitive digestive systems.
Norwegian Kelp, Bladderwrack, and Oarweed—three certified organic sea vegetables—provide alginate fiber, iodine, and trace minerals. These marine botanicals support thyroid function while delivering prebiotic compounds that feed beneficial bacteria. The trace mineral content addresses a frequently overlooked aspect of microbiome health: bacteria require minerals as cofactors for enzymatic functions, and mineral deficiency can limit bacterial growth even when other nutrients are adequate.[55] Learn more about trace minerals' essential role in supporting gut health.
This diverse prebiotic blend ensures that all 26 probiotic strains—not just Bifidobacterium—receive appropriate nutrition for colonization and metabolic activity. The combination creates what scientists call a "permissive environment" where beneficial bacteria can establish, multiply, and exert their health-promoting functions.
Zero Fillers: Every Milligram Serves a Purpose
Perhaps what most distinguishes MicroBiome Restore from conventional probiotics is what it doesn't contain. The formulation includes zero microcrystalline cellulose (wood pulp filler), zero magnesium stearate (manufacturing lubricant), zero silicon dioxide (anti-caking agent), and zero artificial additives of any kind.[57]
This commitment to purity isn't merely marketing—it reflects a fundamental philosophy about supplement formulation. Every milligram of capsule space occupied by fillers and flow agents is a milligram unavailable for therapeutic ingredients. In conventional probiotics, fillers can comprise 20-40% of total capsule content, dramatically diluting the beneficial components consumers are actually purchasing.
By eliminating all excipients, MicroBiome Restore maximizes ingredient density while avoiding substances that research increasingly links to potential gut health concerns. Studies show that silicon dioxide nanoparticles can damage intestinal microvilli and impair nutrient absorption at realistic exposure levels—exactly the opposite of what people taking probiotics are trying to achieve.[58] For detailed analysis of these concerns, read our comprehensive article on microcrystalline cellulose safety issues.
The filler-free approach requires accepting higher manufacturing costs and more complex production processes, but the result is a formulation where literally every ingredient—from the probiotic strains to the organic prebiotics to the pullulan capsule itself—contributes to gut ecosystem restoration. Discover more about why choosing probiotics without microcrystalline cellulose matters.
Pullulan Capsules: Functional Packaging
Even the capsule material in MicroBiome Restore serves dual purpose. Rather than using conventional gelatin or HPMC capsules that function purely as inert containers, the formulation uses pullulan—a plant-based polysaccharide created through fermentation that provides superior oxygen barrier protection (up to 300 times better than HPMC) while serving as a prebiotic substrate.
Research demonstrates that pullulan is selectively fermented by beneficial Lactobacillus and Bifidobacterium species, effectively making the capsule itself nutritional support rather than waste material.[44] Pullulan capsules also dissolve quickly in the stomach, breaking down into short-chain fatty acids that promote activity of beneficial bacteria. This represents the kind of thoughtful formulation detail that separates premium products from mass-market alternatives.
Practical Strategies for Supporting Bifidobacterium Levels
While probiotic supplementation offers targeted support for Bifidobacterium restoration, comprehensive gut health requires a multifaceted approach incorporating dietary choices, lifestyle factors, and strategic supplementation.

Dietary Foundations: Fiber and Fermented Foods
The single most important dietary factor for supporting Bifidobacterium is adequate fiber intake—specifically the types of fiber that these bacteria preferentially ferment. Aim for 25-35 grams of total fiber daily from diverse plant sources including whole grains, legumes, vegetables, fruits, nuts, and seeds.[59]
Particularly beneficial fiber sources include:
Resistant starch found in cooked and cooled potatoes, rice, and beans—this unique starch resists digestion in the small intestine and reaches the colon intact where Bifidobacterium species ferment it into beneficial metabolites. Resistant starch has been shown to selectively increase Bifidobacterium abundance while improving insulin sensitivity and reducing inflammation.[60]
Inulin-rich foods including chicory root, garlic, onions, leeks, asparagus, and bananas provide the fructan prebiotics that Bifidobacterium preferentially consume. Start with small amounts if you're not accustomed to these foods, as rapid increases can cause temporary digestive discomfort while your microbiome adapts.
Beta-glucans from oats, barley, and medicinal mushrooms support both Bifidobacterium growth and immune function. These unique polysaccharides show bifidogenic properties—they specifically promote Bifidobacterium proliferation more than other bacterial groups.[61]
Fermented foods provide both probiotic bacteria and the metabolites these bacteria produce during fermentation. While most fermented foods don't contain Bifidobacterium (which requires anaerobic conditions and milk-based substrates), foods like yogurt, kefir, sauerkraut, kimchi, and kombucha introduce other beneficial bacteria and create gut environments more hospitable to Bifidobacterium colonization.[62] Explore natural food sources of probiotics for more dietary guidance.
Limiting Antibiotic Exposure
Given antibiotics' devastating impact on Bifidobacterium populations, judicious use is critical. Antibiotics remain life-saving medications for bacterial infections, but they're frequently overprescribed for viral conditions where they provide no benefit while decimating gut microbiota.[63]
When antibiotics are medically necessary, consider probiotic supplementation during and after treatment to help mitigate microbiome damage and speed recovery. While taking probiotics simultaneously with antibiotics was once discouraged due to concerns about antibiotic killing of probiotic bacteria, research now suggests that certain robust strains (particularly soil-based organisms and Saccharomyces boulardii) can survive antibiotic exposure and provide benefits even during treatment.[64]
After completing antibiotic courses, extended probiotic supplementation (2-3 months minimum) can help restore Bifidobacterium populations and prevent long-term dysbiosis. The longer antibiotics are taken and the broader their spectrum, the more important post-antibiotic restoration becomes.
Managing Stress and Supporting Circadian Rhythms
The gut-brain axis means that psychological stress directly impacts gut microbiome composition, with Bifidobacterium showing particular vulnerability to chronic stress. Studies demonstrate that stress hormones alter intestinal motility, mucus production, and immune function in ways that reduce Bifidobacterium abundance.[19]
Stress management techniques including regular exercise, adequate sleep, meditation, and social connection don't just improve mental health—they create gut environments more favorable for beneficial bacteria. Even moderate exercise has been shown to increase Bifidobacterium abundance independent of dietary changes.[65] Learn about the bidirectional relationship between gut health and athletic performance.
Circadian rhythm disruption from shift work, jet lag, or irregular sleep schedules also negatively impacts gut microbiota including Bifidobacterium. These bacteria follow diurnal rhythmic patterns synchronized with host feeding and activity cycles. Chronic circadian disruption desynchronizes these patterns, potentially contributing to metabolic dysfunction and inflammation.[66] Maintaining consistent sleep-wake schedules and regular meal timing supports microbiome stability.
Strategic Supplementation Timing and Approach
For optimal results with probiotic supplementation, consider timing and administration details:
Take probiotics consistently—beneficial effects accumulate with regular use over weeks to months rather than appearing immediately. Most clinical studies showing health benefits use supplementation periods of 4-12 weeks minimum. Bifidobacterium colonization and ecosystem remodeling takes time.
Consider taking with meals—while some sources recommend taking probiotics on an empty stomach, research shows that food buffers stomach acid and improves bacterial survival through the gastric environment. The protective effect of food may outweigh any theoretical advantage of faster gastric emptying on an empty stomach.[67] Read our detailed guide on the best time to take probiotics for maximum benefit.
Start gradually if you have sensitive digestion—while high-quality probiotics are generally well-tolerated, individuals with compromised gut health may experience temporary changes in bowel habits, mild bloating, or digestive adjustment during the first 1-2 weeks. Starting with a half dose and gradually increasing allows your system to adapt.
Pair with prebiotic-rich foods—even when taking synbiotic supplements that include prebiotics, dietary fiber remains critically important. The combination of supplemental probiotics, supplemental prebiotics, and dietary fiber provides maximum support for Bifidobacterium restoration.
Track your response—keep notes on digestive symptoms, energy levels, mood, sleep quality, and any health concerns you're addressing. This helps you evaluate whether the specific formulation is providing benefits and whether adjustments might be needed. Remember that individual microbiome differences mean responses to probiotics vary—what works optimally for one person may differ from what another person needs.
Comprehensive Protocol Approaches
For individuals dealing with significant gut dysbiosis, comprehensive protocols combining multiple interventions offer the best outcomes. The Gut Essentials Protocol from BioPhysics Essentials combines MicroBiome Restore with X-Cellerator Full Spectrum Minerals to address both microbial restoration and the mineral deficiencies that can limit bacterial growth and metabolic function.
This protocol approach recognizes that gut health exists within a broader metabolic and nutritional context. Bacteria require trace minerals as enzyme cofactors, and mineral deficiency—common in modern diets—can limit the benefits of even high-quality probiotic supplementation.[68] By addressing both microbial populations and mineral status simultaneously, comprehensive protocols accelerate restoration and optimize long-term outcomes.
The Future of Bifidobacterium Research and Microbiome Medicine
Our understanding of Bifidobacterium's role in human health continues evolving rapidly as research methodologies advance and large-scale population studies like the My Baby Biome project generate unprecedented data. Several emerging areas promise to deepen our knowledge and improve clinical applications:
Strain-Specific Mechanisms and Precision Probiotics
While we know different Bifidobacterium species perform distinct functions, research is now elucidating strain-level differences within species. Not all B. longum strains, for instance, show identical metabolic capabilities or immunomodulatory properties. Advanced genomic analysis reveals substantial genetic diversity even among strains of the same species, with this diversity translating into functional differences.[69]
This knowledge enables more precise probiotic selection targeting specific health conditions. Future formulations may match particular Bifidobacterium strains to individual microbiome profiles and health goals—truly personalized probiotic medicine rather than one-size-fits-all approaches.
Metabolite-Based Therapeutics
Rather than delivering live bacteria, an emerging approach focuses on providing the beneficial metabolites that healthy Bifidobacterium populations produce—particularly short-chain fatty acids like acetate and butyrate, or specific bacterial proteins that interact with host immune receptors. This "postbiotic" approach bypasses challenges of bacterial viability and colonization while delivering therapeutic compounds directly.[70]
However, whole bacteria likely provide benefits beyond identified metabolites through complex ecological interactions that isolated compounds cannot replicate. The future probably involves both approaches—live probiotics for ecosystem restoration and targeted metabolites for specific therapeutic effects.
Early Life Interventions and Prevention
Given the critical importance of early Bifidobacterium colonization for immune development and disease prevention, research is exploring interventions to ensure optimal infant microbiome establishment. Maternal probiotic supplementation during pregnancy and breastfeeding, immediate post-birth Bifidobacterium administration to C-section infants, and optimized infant formula supplementation all show promise for reducing the 25% deficiency rate observed in U.S. infants.[71]
Some researchers propose universal newborn microbiome screening to identify at-risk infants before health problems develop, enabling early interventions that might prevent allergic and autoimmune conditions. While regulatory and practical challenges remain, the preventive potential of ensuring adequate early-life Bifidobacterium is enormous.
Microbiome-Directed Therapies for Specific Diseases
Clinical trials are investigating Bifidobacterium supplementation for specific conditions ranging from colorectal cancer prevention to cognitive decline in elderly populations. Early results suggest targeted applications may offer benefits beyond general gut health support.[72]
As mechanisms become better understood, we can expect more condition-specific probiotic formulations—perhaps Bifidobacterium strains selected for metabolic support in diabetes, different strains optimized for immune modulation in autoimmune disease, and still others targeted for cognitive and mood support through gut-brain axis mechanisms.
Conclusion: Restoring the Missing Foundation of Gut Health
The widespread deficiency of Bifidobacterium affecting approximately one quarter of U.S. infants—and persisting through adulthood as natural age-related decline compounds early-life deficits—represents one of the most significant public health challenges of our time. These beneficial bacteria aren't optional accessories to human health; they're fundamental components of our biology that evolved alongside us over hundreds of thousands of years.
When Bifidobacterium populations are absent or depleted, the consequences ripple throughout body systems: immune dysfunction manifesting as allergies and autoimmune conditions, metabolic disruption contributing to obesity and diabetes, cognitive and mood impacts affecting mental health and brain aging, inflammatory activation accelerating chronic disease, and reduced infection resistance compromising acute illness responses. The My Baby Biome study's finding that Bifidobacterium-deficient infants face three-fold increased risk of atopic disease by age two represents just the tip of the iceberg—the early warning of broader health impacts that may persist lifelong.
Severe gut dysbiosis, including small intestinal bacterial overgrowth (SIBO), often accompanies Bifidobacterium deficiency—and clinical research shows specific B. lactis strains can help address both issues.
Yes, this challenge is solvable. Unlike genetic diseases where intervention options remain limited, microbiome deficiency responds to targeted restoration strategies. Multi-strain probiotic supplementation providing diverse Bifidobacterium species—B. longum, B. lactis, B. breve, B. infantis, and B. bifidum—alongside complementary beneficial bacteria, organic prebiotics to feed these microbes, essential trace minerals, and advanced delivery technology offers comprehensive support for rebuilding depleted microbiomes.
The formulation approach matters tremendously. Conventional probiotics often prioritize manufacturing convenience over therapeutic efficacy, filling capsules with inert fillers and flow agents that waste valuable space while potentially compromising gut health. Premium formulations like MicroBiome Restore take the opposite approach—maximizing ingredient density, eliminating all excipients, incorporating diverse organic prebiotics, and using functional capsule materials that themselves support beneficial bacteria.
Beyond supplementation, supporting Bifidobacterium requires addressing the broader factors driving modern deficiency: prioritizing vaginal birth when medically safe, using antibiotics judiciously and restoring microbiomes after necessary courses, consuming fiber-rich whole food diets, managing stress effectively, maintaining regular sleep-wake cycles, and minimizing exposure to factors that disrupt gut ecosystems. These lifestyle foundations create permissive environments where Bifidobacterium can establish, thrive, and exert their manifold health-promoting functions.
As research continues elucidating Bifidobacterium's roles in human health—from infancy through old age, from digestive function through brain health—the imperative for restoration becomes ever clearer. We cannot afford to ignore the missing microbes that form the foundation of properly functioning gut ecosystems. Whether you're concerned about infant microbiome development, addressing adult digestive issues, or supporting healthy aging, ensuring adequate Bifidobacterium represents one of the most evidence-based interventions available.
The good news is that even individuals with long-standing deficiency can benefit from restoration. The microbiome retains remarkable plasticity—the capacity to reshape itself given appropriate inputs. Consistent probiotic supplementation combined with prebiotic nutrition and supportive lifestyle factors can substantially increase Bifidobacterium abundance over weeks to months, bringing with it improvements in immune function, metabolic health, digestive comfort, and systemic wellbeing.
Your gut microbiome is not destiny—it's a dynamic ecosystem you can actively support and optimize. Understanding Bifidobacterium deficiency and implementing targeted restoration strategies empowers you to take control of this fundamental aspect of health. The missing microbes can be restored, the depleted ecosystem can be rebuilt, and the health consequences can be reversed. It starts with recognizing the problem and choosing interventions—both supplemental and lifestyle—that provide comprehensive support rather than superficial solutions.
For evidence-based Bifidobacterium restoration without fillers, excipients, or compromises, explore MicroBiome Restore or learn about our comprehensive Gut Essentials Protocol for complete microbiome and metabolic support.
References
- Jarman, J. B., et al. (2025). "Bifidobacterium deficit in United States infants drives prevalent gut dysbiosis." Communications Biology, 8(1), 867. https://www.nature.com/articles/s42003-025-08274-7
- Medical Xpress. (2025). "Missing beneficial bacteria in infant guts linked to rising asthma and allergy cases." https://medicalxpress.com/news/2025-07-beneficial-bacteria-infant-guts-linked.html
- Arboleya, S., et al.(2016). "Gut Bifidobacteria Populations in Human Health and Aging." Frontiers in Microbiology, 7, 1204. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4990546/
- Gavzy, S. J., et al. (2023). "Bifidobacterium mechanisms of immune modulation and tolerance." Gut Microbes, 15(2), 2291164. https://pmc.ncbi.nlm.nih.gov/articles/PMC10730214/
- Turroni, F., et al. (2017). "Bifidobacteria and Their Health-Promoting Effects." Microbiology Spectrum, 5(3). https://journals.asm.org/doi/10.1128/microbiolspec.bad-0010-2016
- Pokusaeva, K., et al. (2011). "Carbohydrate metabolism in Bifidobacteria." Genes & Nutrition, 6(3), 285-306. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3145055/
- Turroni, F., et al. (2018). "The infant gut microbiome as a microbial organ influencing host well-being." Italian Journal of Pediatrics, 44(Suppl 1), 16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5833078/
- O'Callaghan, A., & van Sinderen, D. (2016). "Bifidobacteria and Their Role as Members of the Human Gut Microbiota." Frontiers in Microbiology, 7, 925. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4908950/
- Saturio, S., et al. (2023). "Role of Bifidobacteria on Infant Health." Microorganisms, 11(12), 2896. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10744262/
- Huda, M. N., et al. (2019). "Bifidobacterium abundance in early infancy and vaccine response at 2 years of age." Pediatrics, 143(2), e20181489. https://pubmed.ncbi.nlm.nih.gov/30670586/
- Odamaki, T., et al. (2016). "Age-related changes in gut microbiota composition from newborn to centenarian: a cross-sectional study." BMC Microbiology, 16, 90. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4861297/
- Taft, D. H., et al. (2022). "Bifidobacterium species colonization in infancy: a global cross-sectional comparison by population history of breastfeeding." Nutrients, 14(7), 1423. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9003218/
- Lange, K., et al. (2016). "Effects of antibiotics on gut microbiota." Digestive Diseases, 34(3), 260-268. https://pubmed.ncbi.nlm.nih.gov/27028893/
- Davis, E. C., et al. (2024). "Gut microbiome in the first 1000 days and risk for childhood food allergy." Annals of Allergy, Asthma & Immunology, 133(3), 252-261. https://pubmed.ncbi.nlm.nih.gov/38821380/
- Borewicz, K., et al. (2019). "The effect of prebiotic fortified infant formulas on microbiota composition and dynamics in early life." Scientific Reports, 9, 2434. https://www.nature.com/articles/s41598-018-38268-x
- Quagliani, D., & Felt-Gunderson, P. (2017). "Closing America's Fiber Intake Gap: Communication Strategies From a Food and Fiber Summit." American Journal of Lifestyle Medicine, 11(1), 80-85. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6124841/
- Rook, G., & Rosa Brunet, L. (2005). "Old friends for breakfast." Clinical & Experimental Allergy, 35(6), 841-842. https://pubmed.ncbi.nlm.nih.gov/15969656/
- Seppo, A. E., et al. (2021). "Infant gut microbiome is enriched with Bifidobacterium longum ssp. infantis in old order mennonites with traditional farming lifestyle." Allergy, 76(11), 3489-3503. https://pubmed.ncbi.nlm.nih.gov/33955566/
- Madison, A., & Kiecolt-Glaser, J. K. (2019). "Stress, depression, diet, and the gut microbiota: human-bacteria interactions at the core of psychoneuroimmunology and nutrition." Current Opinion in Behavioral Sciences, 28, 105-110. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6874441/
- Koh, A., et al. (2016). "From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites." Cell, 165(6), 1332-1345. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4884116/
- Dong, P., et al. (2018). "A low abundance of Bifidobacterium but not Lactobacillus in the feces of Chinese children with wheezing diseases." Medicine, 97(35), e12029. https://journals.lww.com/md-journal/fulltext/2018/08310/a_low_abundance_of_bifidobacterium_but_not.29.aspx
- Png, C. W., et al. (2010). "Mucolytic bacteria with increased prevalence in IBD mucosa augment in vitro utilization of mucin by other bacteria." American Journal of Gastroenterology, 105(11), 2420-2428. https://pubmed.ncbi.nlm.nih.gov/20648002/
- Mirza, A., & Mao-Draayer, Y. (2017). "The gut microbiome and microbial translocation in multiple sclerosis." Clinical Immunology, 183, 213-224. https://pubmed.ncbi.nlm.nih.gov/28723401/
- Shang, Q., et al. (2021). "Gut Microbiota Fermentation of Marine Polysaccharides and Its Effects on Intestinal Ecology: An Overview." Carbohydrate Polymers, 251, 117064. https://pubmed.ncbi.nlm.nih.gov/33142595/
- Canfora, E. E., et al. (2015). "Short-chain fatty acids in control of body weight and insulin sensitivity." Nature Reviews Endocrinology, 11(10), 577-591. https://pubmed.ncbi.nlm.nih.gov/26260141/
- Aoki, R., et al. (2017). "Commensal microbe-derived acetate suppresses NAFLD/NASH development via hepatic FFAR2 signaling in mice." Microbiome, 5, 144. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5688671/
- Cryan, J. F., et al. (2019). "The Microbiota-Gut-Brain Axis." Physiological Reviews, 99(4), 1877-2013. https://pubmed.ncbi.nlm.nih.gov/31460832/
- Ng, Q. X., et al. (2018). "A meta-analysis of the use of probiotics to alleviate depressive symptoms." Journal of Affective Disorders, 228, 13-19. https://pubmed.ncbi.nlm.nih.gov/29232559/
- Ticinesi, A., et al. (2019). "Gut microbiota, cognitive frailty and dementia in older individuals: a systematic review." Clinical Interventions in Aging, 14, 1497-1511. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6715825/
- Yeoh, Y. K., et al. (2021). "Lost microbes of COVID-19: Bifidobacterium, Faecalibacterium depletion and decreased microbiome diversity associated with SARS-CoV-2 infection severity." BMJ Open Gastroenterology, 8(1), e000601. https://pmc.ncbi.nlm.nih.gov/articles/PMC9051551/
- Wickramasinghe, S., et al. (2024). "Bifidobacterium: Host-Microbiome Interaction and Mechanism of Action in Preventing Common Gut-Microbiota-Associated Complications in Preterm Infants." Nutrients, 15(3), 709. https://www.mdpi.com/2072-6643/15/3/709
- Liao, W., et al. (2025). "Bifidobacterium depletion promotes goiter via gut-thyroid axis: evidence from Mendelian randomization and experimental validation." Frontiers in Microbiology, 16, 1621167. https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1621167/full
- Lawson, M. A. E., et al. (2020). "Breast milk-derived human milk oligosaccharides promote Bifidobacterium interactions within a single ecosystem." ISME Journal, 14(2), 635-648. https://www.nature.com/articles/s41396-019-0553-2
- Milani, C., et al. (2017). "Exploring Bifidobacterium species community and functional variations with human gut microbiome structure and health beyond infancy." Microbiome Research Reports, 2, 7. https://www.oaepublish.com/articles/mrr.2023.01
- Morovic, W., et al. (2016). "Transcriptional and functional analysis of Bifidobacterium animalis subsp. lactis exposure to tetracycline." Applied and Environmental Microbiology, 82(20), 6145-6154. https://pubmed.ncbi.nlm.nih.gov/27496773/
- Martin, R., et al. (2010). "Human milk is a source of lactic acid bacteria for the infant gut." Journal of Pediatrics, 143(6), 754-758. https://pubmed.ncbi.nlm.nih.gov/14657823/
- Turroni, F., et al. (2014). "Bifidobacterium bifidum PRL2010 modulates the host innate immune response." Applied and Environmental Microbiology, 80(2), 730-740. https://pubmed.ncbi.nlm.nih.gov/24242251/
- Chapman, C. M. C., et al. (2011). "Health benefits of probiotics: are mixtures more effective than single strains?" European Journal of Nutrition, 50(1), 1-17. https://pubmed.ncbi.nlm.nih.gov/21229254/
- Gibson, G. R., et al. (2017). "Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics." Nature Reviews Gastroenterology & Hepatology, 14(8), 491-502. https://pubmed.ncbi.nlm.nih.gov/28611480/
- Cherbut, C., et al. (2003). "Acacia gum is a bifidogenic dietary fibre with high digestive tolerance in healthy humans." Microbial Ecology in Health and Disease, 15(1), 43-50. https://www.tandfonline.com/doi/abs/10.1080/08910600310014377
- Jayachandran, M., et al. (2017). "A critical review on the impacts of β-glucans on gut microbiota and human health." Journal of Nutritional Biochemistry, 61, 101-110. https://pubmed.ncbi.nlm.nih.gov/30196242/
- Sibanda, T., et al. (2024). "Bifidobacterium species viability in dairy-based probiotic foods: challenges and innovative approaches." Frontiers in Microbiology, 15, 1327010. https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1327010/full
- Moreton, R. C. (2009). "Capsule technologies: An overview." American Pharmaceutical Review, 12(4), 54-58.
- Li, W., et al. (2019). "Pullulan nanoparticles as prebiotics enhance the antibacterial properties of Lactobacillus plantarum through the induction of mild stress in probiotics." Frontiers in Microbiology, 10, 142. https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2019.00142/full
- Ishizeki, S., et al. (2013). "Effect of administration of bifidobacteria on intestinal microbiota in low-birth-weight infants and transition of administered bifidobacteria: a comparison between one-species and three-species administration." Anaerobe, 23, 38-44. https://pubmed.ncbi.nlm.nih.gov/23933096/
- Jungersen, M., et al. (2014). "The Science behind the Probiotic Strain Bifidobacterium animalis subsp. lactis BB-12." Microorganisms, 2(2), 92-110. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5029497/
- Enomoto, T., et al. (2014). "Effects of bifidobacterial supplementation to pregnant women and infants in the prevention of allergy development in infants and on fecal microbiota." Allergology International, 63(4), 575-585. https://pubmed.ncbi.nlm.nih.gov/25056226/
- Henrick, B. M., et al. (2021). "Bifidobacterium-mediated immune system imprinting early in life." Cell, 184(15), 3884-3898. https://pubmed.ncbi.nlm.nih.gov/34242577/
- Guglielmetti, S., et al. (2011). "Randomised clinical trial: Bifidobacterium bifidum MIMBb75 significantly alleviates irritable bowel syndrome and improves quality of life." Alimentary Pharmacology & Therapeutics, 33(10), 1123-1132. https://pubmed.ncbi.nlm.nih.gov/21418261/
- Probiotic strains in MicroBiome Restore formulation. BioPhysics Essentials product documentation.
- Elshaghabee, F. M. F., et al. (2017). "Bacillus As Potential Probiotics: Status, Concerns, and Future Perspectives." Frontiers in Microbiology, 8, 1490. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5544598/
- Niness, K. R. (1999). "Inulin and oligofructose: what are they?" Journal of Nutrition, 129(7 Suppl), 1402S-1406S. https://pubmed.ncbi.nlm.nih.gov/10395607/
- Maftoun, P., et al. (2015). "Optimization of immune-modulatory effects of Maitake mushroom on adjuvanticity in avian influenza H9N2 vaccine." Veterinary Research Forum, 6(3), 215-221. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4666852/
- Calame, W., et al. (2008). "Gum arabic establishes prebiotic functionality in healthy human volunteers in a dose-dependent manner." British Journal of Nutrition, 100(6), 1269-1275. https://pubmed.ncbi.nlm.nih.gov/18466655/
- Zoroddu, M. A., et al. (2019). "The essential metals for humans: a brief overview." Journal of Inorganic Biochemistry, 195, 120-129. https://pubmed.ncbi.nlm.nih.gov/30939379/
- MicroBiome Restore ingredient label and formulation specifications. BioPhysics Essentials.
- Guo, Z., et al. (2018). "Silicon dioxide nanoparticle exposure affects small intestine function in an in vitro model." Nanotoxicology, 12(5), 485-508. https://pmc.ncbi.nlm.nih.gov/articles/PMC6157813/
- Deehan, E. C., & Walter, J. (2016). "The Fiber Gap and the Disappearing Gut Microbiome: Implications for Human Nutrition." Trends in Endocrinology & Metabolism, 27(5), 239-242. https://pubmed.ncbi.nlm.nih.gov/27079516/
- Bindels, L. B., et al. (2017). "Resistant starch can improve insulin sensitivity independently of the gut microbiota." Microbiome, 5, 12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5259860/
- El Khoury, D., et al. (2012). "Beta glucan: health benefits in obesity and metabolic syndrome." Journal of Nutrition and Metabolism, 2012, 851362. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3236515/
- Marco, M. L., et al. (2021). "The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on fermented foods." Nature Reviews Gastroenterology & Hepatology, 18(3), 196-208. https://pubmed.ncbi.nlm.nih.gov/33239795/
- Yassour, M., et al. (2016). "Natural history of the infant gut microbiome and impact of antibiotic treatment on bacterial strain diversity and stability." Science Translational Medicine, 8(343), 343ra81. https://pubmed.ncbi.nlm.nih.gov/27306664/
- McFarland, L. V. (2015). "From Yaks to Yogurt: The History, Development, and Current Use of Probiotics." Clinical Infectious Diseases, 60(Suppl 2), S85-S90. https://pubmed.ncbi.nlm.nih.gov/25922408/
- Allen, J. M., et al. (2018). "Exercise Alters Gut Microbiota Composition and Function in Lean and Obese Humans." Medicine & Science in Sports & Exercise, 50(4), 747-757. https://pubmed.ncbi.nlm.nih.gov/29166320/
- Voigt, R. M., et al. (2016). "The Circadian Clock Mutation Promotes Intestinal Dysbiosis." Alcoholism: Clinical and Experimental Research, 40(2), 335-347. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4724313/
- Tompkins, T. A., et al. (2011). "The impact of meals on a probiotic during transit through a model of the human upper gastrointestinal tract." Beneficial Microbes, 2(4), 295-303. https://pubmed.ncbi.nlm.nih.gov/22146689/
- Borch-Iohnsen, B. (1993). "Influence of essential mineral elements on the gut microbiota." Microbial Ecology in Health and Disease, 6(6), 307-315.
- Lugli, G. A., et al. (2019). "Comparative genomic and phylogenomic analyses of the Bifidobacteriaceae family." BMC Genomics, 18, 568.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5513268/
- Aguilar-Toalá, J. E., et al. (2024). "Compendium of Bifidobacterium-based probiotics: characteristics and therapeutic impact on human diseases." Microbiome Research Reports, 3(4), 52. https://www.oaepublish.com/articles/mrr.2024.52
- Milani, C., et al. (2017). "The First Microbial Colonizers of the Human Gut: Composition, Activities, and Health Implications of the Infant Gut Microbiota." Microbiology and Molecular Biology Reviews, 81(4), e00036-17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5706746/
- Hibberd, A. A., et al. (2017). "Intestinal microbiota is altered in patients with colon cancer and modified by probiotic intervention." BMJ Open Gastroenterology, 4(1), e000145. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5531274/
Legal Disclaimer: The statements made on this page have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease. The information provided is for educational purposes only and is not intended as a substitute for advice from your physician or other healthcare professional. You should not use the information on this site for diagnosis or treatment of any health problem or for prescription of any medication or other treatment. Always consult with a healthcare professional before starting any diet, exercise, or supplementation program, before taking any medication, or if you have or suspect you might have a health problem. Individual results may vary.



Share and get 15% off!
Simply share this product on one of the following social networks and you will unlock 15% off!